Gurmeet Singh, Gursharan Singh, Sunita Arora.
Department of Paediatrics, Sh Guru Ram Das Institute of Medical Sciences & Research, Vallah, Amritsar, Punjab, India.
ADDRESS FOR CORRESPONDENCE
Dr Gurmeet Singh, Department of Paediatrics, Sh Guru Ram Das Institute of Medical Sciences & Research, Vallah, Amritsar 143001, Punjab, India.
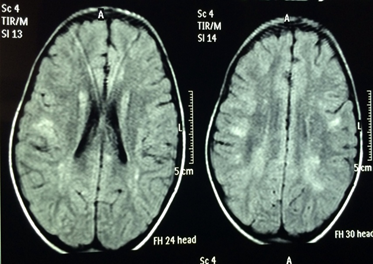
Email: dr.gmsingh@gmail.com | | Keywords | | Dengue infection, complications, encephalomyelitis | | | A six year old boy was hospitalized with four days history of high grade fever, chills, body ache and vomiting. Hemogram showed thrombocytopenia (platelet count 50000/cumm). Dengue NS1 antigen and IgM antibody were positive. There was no active bleeding. He was managed conservatively and discharged after five days. Fever had resolved and platelet counts had improved by then. About two weeks later he was again hospitalized with complaints of inability to walk, weakness in left arm and dribbling of urine. On examination, he had decreased power and tone in affected limbs. Deep tendon reflexes were absent in both lower limbs and left upper limb. Urinary bladder was full and child was able to pass urine only on manual stimulation. There was no sign of meningeal irritation. Other neurological and systemic examinations were normal. After admission, child had single episode of generalized seizure which was managed with midazolam and a loading dose of phenytoin. Cerebrospinal fluid (CSF) examination showed proteins 80 mg%, 75 cells /cumm (predominantly lymphocytes) and normal sugar. MRI brain & spinal cord showed multifocal ill-defined bilateral supratentorial deep as well as subcortical white matter hyperintensities (figure 1) with ill-defined cervical/proximal dorsal cord edema suggestive of acute disseminated encephalomyelitis (ADEM). He was given IV methylprednisolone (30mg/kg/day) for five days and then started on oral prednisolone (1mg/kg/day) for two weeks. He showed dramatic improvement 48 hours after steroids were started and had complete resolution in ten days.
Figure 1: T2 Flair MRI image showing multi focal subcortical hyperintensities.
Dengue fever is caused by four distinct type of RNA viruses (type 1 to 4) that are closely related antigenically belonging to flaviviridae family. Nervous system involvement is seen with serotypes 2&3. (1) Reported incidence of encephalopathy and encephalitis being the most common neurological complications of dengue has been found to vary between 0.5% to 6.2%. (2) Neurological complications of dengue infections can be classified in 3 categories: a) Neurotropic effects of virus resulting in encephalitis, meningitis, myositis & myelitis; b) Systemic complications of dengue manifesting as encephalopathy, stroke or hypokalemic paralysis and c) Post-infectious complications which are mostly immune mediated and include ADEM, Guillian Barre Syndrome (GBS) and optic neuritis etc. (3) Our patient had ADEM due to previous dengue infection. ADEM as a neurological complication has rarely been described in association with dengue in children. (3,4) Pathophysiology involves transient autoimmune response towards myelin or other self-antigens, possibly via molecular mimicry or by nonspecific activation of auto-reactive T-cell clones. (5) Intravenous methyl prednisolone (10–30 mg/kg/day, up to a maximum of 1 g/day) for 3–5 days is being used as first line drug. (4) It has been seen that recovery is incomplete in patients of ADEM not receiving any form of immune modulation treatment (high dose methylprednisolone, ivig or plasmapheresis). (4) Our patient had a good response to methyl prednisolone. | | | | Compliance with Ethical Standards | | Funding None | | | | Conflict of Interest None | | |
- Karoli R, Siddiqi Z, Fatima J, Maini S. Was it a case of acute disseminated encephalomyelitis? A rare association following dengue fever. J Neurosci Rural Pract 2013; 4: 318-21. [CrossRef] [PMC free article]
- Hendarto SK, Hadinegoro SR. Dengue encephalopathy. Acta Paediatr Jpn 1992; 34: 350-7. [CrossRef]
- Murthy JM. Neurological complication of dengue infection. Neurol India 2010; 58: 581-4. [CrossRef]
- Alexander M, Murthy JM. Acute disseminated encephalomyelitis: treatment guidelines. Ann Indian Acad Neurol 2011; 14: 560-4. [CrossRef] [PMC free article]
- Murthy JM. Acute disseminated encephalomyelitis. Neurol India 2002; 50: 238-43. [PubMed]
DOI: https://doi.org/10.7199/ped.oncall.2015.8
|
| Cite this article as: | | Singh G, Singh G, Arora S. Acute Disseminated Encephalomyelitis Following Dengue Infection. Pediatr Oncall J. 2015;12: 20. doi: 10.7199/ped.oncall.2015.8 |
|