Nitika Tulsi, Seema Sharma, Neha Rehalia, Milap Sharma.
Deparment of Pediatrics, Dr Rajendra Prasad Government Medical College Kangra, Tanda, Himachal Pradesh, India.
ADDRESS FOR CORRESPONDENCE
Neha Rehalia, Department of Paediatrics, DR RPGMC Tanda at kangra, Himachal Pradesh, India. PIN -176001.
Email: drneharehalia1613@gmail.com | | Abstract | Objective: A prospective study was conducted in a tertiary care centre in north-west India, to determine the status of vitamin D levels and associated risk factors in severe acute malnutrition in children up to 60 months of age.
Methods: Study was done over a period of one year, hundred patients of severe acute malnutrition (SAM) admitted in our tertiary care centre, fulfilling the inclusion criteria were enrolled in the study. After detailed history and examination, patients were evaluated for calcium, phosphorus, alkaline phosphatase and vitamin D levels.
Results: Vitamin D levels were <20 ng/ml in 58% of all studied children, out of which 28% children had inadequate and 30% had deficient levels. Co-relation of vitamin D deficiency (VDD) in SAM patients with various risk factors like age, previous hospitalization, not giving exclusive breastfeeding, protein deficit and lower socioeconomic status were found to be statistically significant.
Conclusion: High prevalence of VDD in patients of SAM needs active surveillance and management. | | | | Keywords | | Vitamin D, severe acute malnutrition, children. | | | | Introduction | Childhood malnutrition is an important public health and development challenge in India. Malnourished children have a significantly higher risk of mortality and morbidity. In addition to increasing the risk of disease and death, malnutrition also causes stunted growth and impaired psychosocial and cognitive development. Severe Acute Malnutrition (SAM) is defined as the presence of severe wasting (weight for height <-3 SD) or mid-upper arm circumference (MUAC) less than or equal to 11.5 cm or bilateral edema.1 Every year million children die before they reach their fifth birthday. Seven out of every ten of these deaths are caused by diarrhoea, pneumonia, measles, malaria or malnutrition.2
SAM children are known to be deficient in vitamins and trace elements.3 SAM children must also have normal skeletal growth and bone health. Calcium and vitamin D are important nutrients for bone growth and bone health.4 Insufficient bone mineralization and disruption of growth plates due to vitamin D and calcium deficiency or phosphate metabolism disorder leads to rickets in children.5
We hypothesized that malnutrition may mask the clinical features of rickets and other biochemical features associated with severe acute malnutrition. With this background we conducted a study to assess the status of vitamin D levels in children with SAM and risk factors associated with vitamin D deficiency (VDD).
Objectives of the study:
To determine status of vitamin D levels and associated risk factors in SAM children up to 60 months of age.
| | | | Methods & Materials | A cross- sectional descriptive study was conducted in the department of Pediatrics, Dr. Rajendra Prasad medical college Kangra at Tanda, Himachal Pradesh in India over one year i.e. from August 2018 to July 2019 after ethical approval from institutional ethical committee. On the basis of study participant selection criteria, 100 i.e. 3.1% of total patients admitted in pediatric ward were enrolled in our study after getting informed written consent from the parents. Enrolled patients were managed as per standard treatment guidelines of SAM.
Selection criteria:
All the children aged up to 60 months getting admitted in the department of Pediatrics, fulfilling any one out of the four criteria for SAM as per World Health Organization (WHO)5 guidelines were included in study. Children with other causes of edema for example; nephrotic syndrome and/or associated systemic diseases, congenital heart disease, mal-absorption, cerebral palsy and who have received mega dose of vitamin D in last six months were excluded.
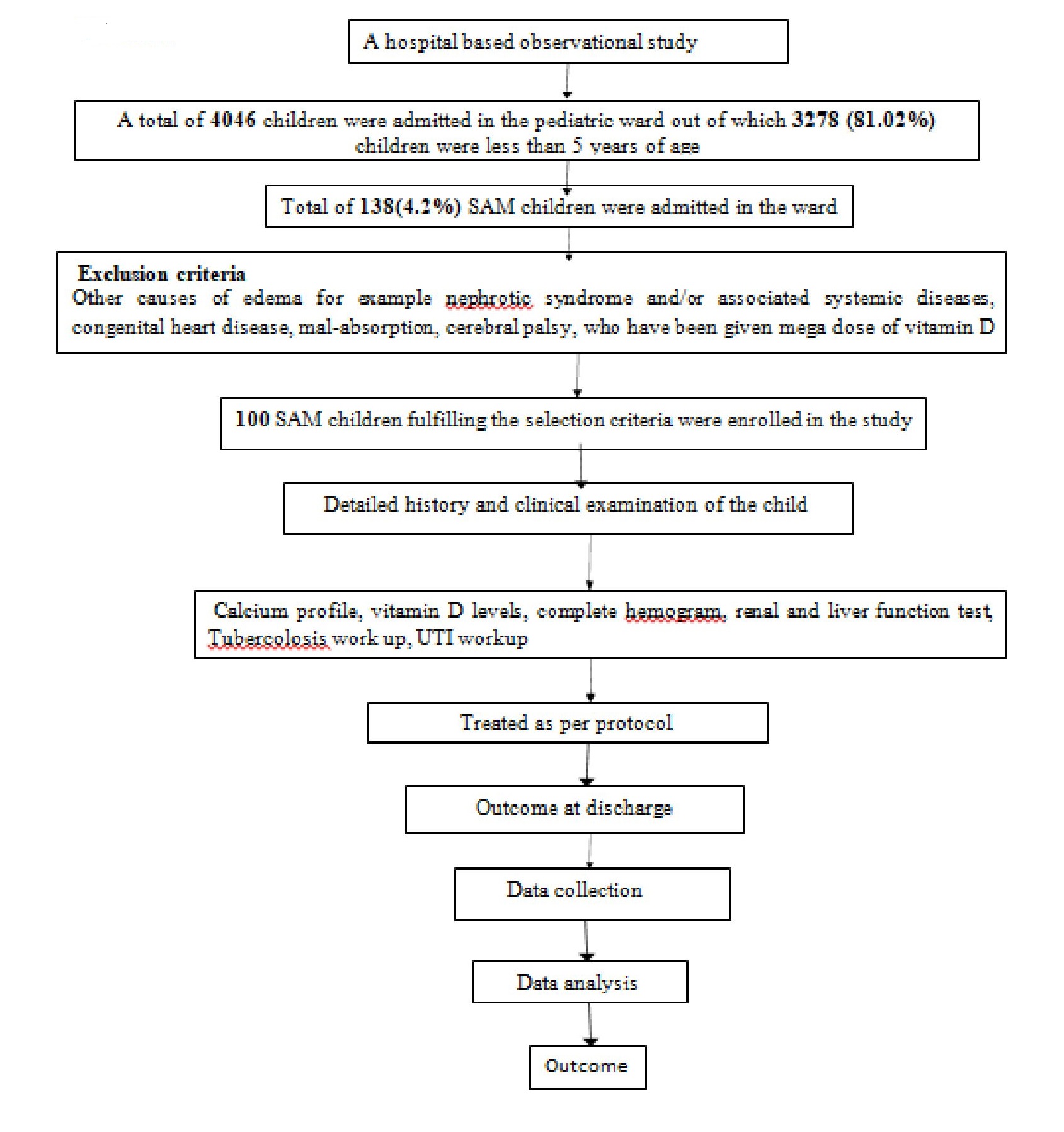
A total of 138 children were screened, 38 were excluded based on our exclusion criteria and finally 100 Children were found eligible according to inclusion criteria. (Figure 1) Detailed history regarding the risk factors and examination of all patients was done. Along with standard set of investigations, all patients were tested for serum calcium, phosphorus, alkaline phosphatase (ALP) and vitamin D levels. Vitamin D levels were done by 5P02 ARCHITECT 25-OH vitamin D reagent kit using electro-chemilumniscense immune assay technique which measure vitamin D concentrations in the range of 0-160 ng/ml. Vitamin D levels ≥20 ng/mL were taken as adequate, 12-20 ng/mL were taken as inadequate and <12 ng/mL were taken as deficiency.
Children were treated as per SAM protocol guidelines and their course of stay was monitored periodically (biweekly) and were discharged as per criterias in WHO Guidelines.6 Data was collected on prescribed precoded performa and was transferred to Microsoft Excel sheet. Microsoft Excel was used in creating the database and producing graphs, while the data was analyzed using Stata software. Percentage, frequency; mean and standard deviation (±SD) were used to describe quantitative data meeting normal distribution. Clinical profile and risk factors for severe acute malnutrition were correlated with vitamin D levels. The level of significance was taken as P <0.05.
Figure 1. Inclusion criteria.
| | | | Results | Out of a total of 3278 children admitted who were less than 5 years of age, 138(4.2%) children were severely acute malnourished. On the basis of study participant selection criteria, 100(3.1%) SAM children were enrolled in our study. Forty seven percent children were under 1 year, followed by 27.0% who were in 13-36 months age group and 26.0% were in >36 months age group; while mean age of studied children was 25.31±20.09 months. Out of 100 patients, 66 were males and 34 were females, with male:female ratio of 2:1 (Table1).
Table 1. Demographic Distribution Of Studied Children.
| Age(Months) |
Frequency(n=100) |
Percentage |
| <12 Months |
47 |
47.0% |
| 13-36 Months |
27 |
27.0% |
| 36 Months |
26 |
26.0% |
| Males |
66 |
66% |
| Females |
34 |
34% |
Failure to gain weight was complaint in all patients, fever in 74.0%, followed by cough in 42.0%, diarrhea in 18.0%, convulsion in 14.0%, lethargy in 10.0%, pallor in 7%, bleeding manifestations in 2 %, generalized body swelling and weight loss in 1.0% each. Sixteen percent of patients had history of previous hospitalization, out of which in 37.5% admissions were due to respiratory illness, followed by diarrhoea, seizure disorder, malnutrition, meningitis & tuberculosis.
During initial six months of life, 55.0% of studied children were on mixed (breast+ top) feeding, 40% were on breast feeding and 5.0% were on top feeding. Out of all children who were not on exclusive in first 6 months of life, diluted cow’s milk (51.6%) was the most common type of milk used, bottle feeding (36.0%) was the most common mode of feeding, but the sterilization technique was improper in all cases. In 8.0% cases complimentary feeding was started before 6 months while 92.0% cases were started on complimentary feeding after 6 months, out of which only 12% were fed as per infant and young child feeding (IYCF) guidelines. All children were found to be calorie deficit and 95% had protein deficit.
Most of the studied children were receiving sufficient time of sunlight exposure in both (summers & winters) seasons and all children were partially covered.
As per modified Kuppuswamy scale, 90.0% children belonged to upper lower class, followed by lower middle (8.0%) and upper middle (2.0%). Thirty nine percent (39%) of the mothers were educated till high school, 35% till intermediate, followed by 15% upto primary/middle school, 6% were illiterate and 5.0% were graduate. Ninety nine percent children utilized anganwadi services.
Eighty two percent (82%) children were small for date (SFD) at birth, while 18% were appropriate for date (AFD). Weight for age was <-3SD in 88% children, weight for height was <-3SD in 100% children; while 22.0% had MUAC ≤11.5 cm, 64% had visible wasting, and 10% had pedal edema. Mean age was 25.31±20.09 months, birth weight was 2.34±0.44 Kg, present weight was 7.41±2.76 Kg, height was 76.50±17.57 cm, occipito-frontal circumference (OFC) was 43.98±4.4cm and MUAC was 12.78±1.83 cm.
Laboratory examination showed evidence of hypocalcaemia in 39%, low phosphorus levels in 16% and high alkaline phosphate levels of >383 U/L in 6% children (Table 2). Vitamin D levels were <20ng/ml in 58% of all studied children, out of which 28% children had inadequate and 30 % had deficient levels (Table 3). Clinical signs of rickets present in 10% of the patients. Co-relation of vitamin D deficiency in SAM patients with various risk factors like age, previous hospitalization, not exclusive breastfeed, protein deficit and lower socioeconomic status, were found to be statistically significant (Table 4).
Table 2. Distribution of Children on Basis of Calcium Profile.
| Calcium Profile |
Frequency(n=100) |
Percentage |
| Calcium Profile |
Hypocalcaemia(<9 mg/dl) |
39 |
39.0 |
| Normal(9-11 mg/dl) |
61 |
61.0 |
| Phosphorus |
Phosphorus Deficient(<4 mg/dl) |
16 |
16.0 |
| Normal(4-7 mg/dl) |
74 |
74.0 |
| Phosphorus Excess(>7 mg/dl) |
9 |
9.0 |
| ALP |
<383 U/L |
94 |
94.0 |
| >383 U/L |
6 |
6.0 |
Table 3. Distribution of Studied Children on the Basis of Vitamin-D Profile.
| Vitamin D |
Frequency(n=100) |
Percentage |
| <12 ng/ml |
Deficiency |
30 |
30.0% |
| 12-20 ng/ml |
Inadequate |
28 |
28.0% |
| >20 ng/ml |
Adequate |
30 |
30.0% |
| >50 ng/ml |
Toxicity |
12 |
12.0% |
Table 4. Risk Factors Associated With Vitamin D Deficiency.
| S. No. |
Risk Factors associated |
Frequency(n=100) |
Vitamin D Deficiency Mean + SD |
P value |
| 1 |
Age |
<12 Months |
47 |
35.44+35.97 |
0.050* |
| 13-36 Months |
27 |
24.99+13.09 |
| >36 Months |
26 |
19.02+8.59 |
| 2 |
Sex |
Male |
66 |
28.44+26.41 |
0.956 |
| Female |
34 |
28.79+28.37 |
| 3 |
Previous Hospitalization |
Yes |
16 |
49.22+44.79 |
0.002* |
| No |
84 |
24.51+20.34 |
| 4 |
Feeding |
Breastfeeding |
40 |
27.99+26.60 |
0.883 |
| Top feeding |
5 |
22.94+16.49 |
| Mixed (breast+top) |
55 |
29.22+28.29 |
| 5 |
Exclusive Breastfeeding |
Given |
40 |
27.99+26.60 |
0.043** |
| Not Given |
60 |
52.16+44.78 |
| 6 |
Milk Dilution |
With dilution |
100 |
30.58+31.41 |
0.530 |
| Without dilution |
0 |
0.0+0.0 |
| 7 |
Complementary Feeding |
After 6 months As per IYCF guidelines |
12 |
29.50+15.19 |
0.598 |
| After 6 months Poor adherence |
80 |
29.11+29.15 |
| Before 6 months |
8 |
17.53+11.13 |
| 8 |
Calorie Deficit |
Yes |
100 |
6.31+11.09 |
- |
| No |
0 |
0.0+0.0 |
| 9 |
Protein Deficit |
Yes |
95 |
28.90+26.90 |
0.024* |
| No |
5 |
4.95+5.44 |
| 10 |
Socioeconomic Status |
Upper Middle |
2 |
84.25+91.57 |
0.010* |
| Lower Middle |
8 |
25.64+14.69 |
| Upper Lower |
90 |
27.11+24.39 |
| 11 |
Maternal Education |
Illiterate |
6 |
23.0+18.44 |
0.803 |
| Primary/Middle school |
15 |
28.86+18.65 |
| High School |
39 |
26.45+24.61 |
| Intermediate |
35 |
32.23+34.41 |
| Graduate |
5 |
18.36+6.68 |
| 12 |
Utilization Of Aganwadi Centre |
Yes |
99 |
28.59+26.89 |
0.421 |
| No |
1 |
6.70+0.0 |
| 13 |
Birth weight |
<2.5 kg |
82 |
30.19+28.80 |
0.175 |
| >2.5 kg |
18 |
19.78+11.94 |
| 14 |
Weight for age |
<-3SD |
88 |
29.31+28.43 |
0.187 |
| >-3SD |
12 |
22.48+13.15 |
| 15 |
Height for age |
<-3SD |
39 |
29.87+27.51 |
0.697 |
| >-3SD |
61 |
27.47+26.67 |
| 16 |
Weight for Height |
<-3SD |
100 |
28.33+26.83 |
- |
| >-3SD |
0 |
0.0+0.00 |
| 17 |
Mid-Upper Arm Circumference (MUAC) |
<11.5cm |
22 |
31.03+41.76 |
0.622 |
| >11.5cm |
78 |
27.54+20.98 |
| | | | Discussion | Nutrition is essential for human development during first five years, it not only affects growth and morbidity, but also determines nutritional status of adolescents and adults. The incidence of SAM was found to be higher in younger children i.e. 74.0% in the children less than 3 years of age. The reason may be the fact that growth and the nutritional needs are maximum in younger age group.7
We found that, the incidence of children under SAM among all hospitalized children was 4.2%. Our findings showed marked increase in prevalence as compared with the study performed by Bhadoria AS et al8 who reported a prevalence of SAM as 2.20%. But prevalence of SAM in our study was lower as compared to national prevalence (7.9%).9 Reason of disparity could be-lower parental education and poor occupation of the head of family predispose a child to SAM. In a similar study from Puducherry by Shewade HD et al10, reported the prevalence of SAM among children from slums in the similar age group (6 months–5 years) as 3.60% and Pravana NK et al11 reported the prevalence of SAM among children under the age of 5 years was 4.14%. So the results of studies done by Shewade HD et al10 and Pravana NK et al11 are comparable with the results of our study.
In the present study, chief complaints of studied children were failure to gain weight in 100%, fever in 74.0%, followed by cough in 42.0%, diarrhea in 18.0%, convulsion in 14.0%, lethargy in 10.0%, pallor in 7%, bleeding manifestations in 2%, generalized body swelling and weight loss in 1.0% each.
Fifty five percent of the studied children were on Mixed (breast+ top) feeding, 40% were on breast feeding and 5.0% were on top feeding in first 6 months of life. Similar findings were reported by Pravana NK et al11 and Prashanth MR et al12 in their respective studies. This showed that feeding practices are not effective and may be a contributory factor for malnutrition.
All the studied patients were found to be calorie deficient and 95% had protein deficit. Prashanth MR et al12 reported calorie deficit in 79.6% and protein deficit in 66.0% patients. There is considerable uncertainty regarding the estimated calorie and protein intakes of breastfed children, and the interpretation of dietary intakes has to be viewed with caution.
Ninety percent children belonged to upper lower class, followed by lower middle (8.0%) and upper middle (2.0%). Pravana NK et al11 reported the majority of their patients of lower group. Studies conducted by Dwivedi et al13 and Avachat et al14 came up with similar inferences. Better socioeconomic conditions are associated with more spending capacity, better living conditions and better-updated knowledge of the parents, hence could result in reduction of malnutrition.
In our study, 39% of the mothers were educated till high school, 35% till intermediate, followed by 15% upto primary/middle school, 6% were illiterate and 5.0% were graduate. Sahoo DP et al15 reported almost the similar data as in present study. It is the fact that mother’s education is associated with the awareness about the proper child-rearing practices, better health-seeking attitude and better knowledge about feeding and immunization.
We found that, 99.0% of the cases have utilized the services of Anganwadi Centre. This showed the health seeking behavior of the studied population, although there was delay in seeking tertiary health care services. This could be because of poor socioeconomic status, difficult terrain and local beliefs and taboos prevailing in our studied population.
In present study 82% children were SFD at the time of birth, while 18% were AFD. Weight for age was <-3SD in 88% children, weight for height was <-3SD in 100% children; while 22.0% had MUAC ≤11.5 cm, 64% had visible wasting, and 10% had pedal edema. Sahoo DP et al15 reported 37.8% of the children were underweight (weight for age) and 14.4% were severely underweight. Stunting (height for age) was present in 37% of the children, and 5.2% were severely stunted. Wasting (weight for age) was present in 35.6% of the children and 14.8% were severely wasted which was similar to the present study. In our study the anthropometric parameters (i.e. W/A, W/H) are more affected as compared to other studies. This could be because of low birth weight, poor socioeconomic status, local beliefs and taboos regarding feeding practices in our studied population.
In our study, 39% of children were hypocalcemic, 16% had low phosphorus levels and 6% had Alkaline e phosphate levels >383U/L. Fifty eight percent of all studied children were having Vitamin D levels<20 ng/ml, out of which 28% children had inadequate and 30% had deficient levels. Prevalence of VDD in malnourished children in study conducted by Mehta S16 was 32%. These findings were similar to those seen in Pakistan (33.6%).17 VDD in children from other countries shows variable prevalence, for instance the prevalence among 12–24 month-olds in China was 65.3%.18 This may be because all other studies had different age groups of children. Our data is comparable to the data from these studies which indicate that VDD is prevalent in SAM children. This could be related to poor nutritional intake, poor sunlight exposure and possibly impaired absorption due of enteric dysfunction or a disease process.
We found that age, previous hospitalization, not giving exclusive breastfeeding, protein calorie deficit and lower socioeconomic status were statistically significant (p<0.05) risk factors associated with vitamin D deficiency in SAM children. There were no such extensive previous studies which showed the association of risk factors in SAM patients having deficiency of vitamin-D. So our study is novel to do the extensive evaluation of association of risk factors in SAM patients having deficiency of vitamin-D.
Nutrition is essential for human development during first five years, it not only affects growth and morbidity, but also determines nutritional status of adolescents and adults. The incidence of SAM was found to be higher in younger children i.e. 74.0% in the children less than 3 years of age. The reason may be the fact that growth and the nutritional needs are maximum in younger age group.7
We found that, the incidence of children under SAM among all hospitalized children was 4.2%. Our findings showed marked increase in prevalence as compared with the study performed by Bhadoria AS et al8 who reported a prevalence of SAM as 2.20%. But prevalence of SAM in our study was lower as compared to national prevalence (7.9%).9 Reason of disparity could be-lower parental education and poor occupation of the head of family predispose a child to SAM. In a similar study from Puducherry by Shewade HD et al10, reported the prevalence of SAM among children from slums in the similar age group (6 months–5 years) as 3.60% and Pravana NK et al11 reported the prevalence of SAM among children under the age of 5 years was 4.14%. So the results of studies done by Shewade HD et al10 and Pravana NK et al11 are comparable with the results of our study.
In the present study, chief complaints of studied children were failure to gain weight in 100%, fever in 74.0%, followed by cough in 42.0%, diarrhea in 18.0%, convulsion in 14.0%, lethargy in 10.0%, pallor in 7%, bleeding manifestations in 2%, generalized body swelling and weight loss in 1.0% each.
Fifty five percent of the studied children were on Mixed (breast+ top) feeding, 40% were on Breast feeding and 5.0% were on top feeding in first 6 months of life. Similar findings were reported by Pravana NK et al11 and Prashanth MR et al12 in their respective studies. This showed that feeding practices are not effective and may be a contributory factor for malnutrition.
All the studied patients were found to be calorie deficient and 95% had protein deficit. Prashanth MR et al12 reported calorie deficit in 79.6% and protein deficit in 66.0% patients. There is considerable uncertainty regarding the estimated calorie and protein intakes of breastfed children, and the interpretation of dietary intakes has to be viewed with caution.
Ninety percent children belonged to upper lower class, followed by lower middle (8.0%) and upper middle (2.0%). Pravana NK et al11 reported the majority of their patients of lower group. Studies conducted by Dwivedi et al13 and Avachat et al14 came up with similar inferences. Better socioeconomic conditions are associated with more spending capacity, better living conditions and better-updated knowledge of the parents, hence could result in reduction of malnutrition.
In our study, 39% of the mothers were educated till high school, 35% till intermediate, followed by 15% upto primary/middle school, 6% were illiterate and 5.0% were graduate. Sahoo DP et al15 reported almost the similar data as in present study. It is the fact that mother’s education is associated with the awareness about the proper child-rearing practices, better health-seeking attitude and better knowledge about feeding and immunization.
We found that, 99.0% of the cases have utilized the services of Anganwadi Centre. This showed the health seeking behavior of the studied population, although there was delay in seeking tertiary health care services. This could be because of poor socioeconomic status, difficult terrain and local beliefs and taboos prevailing in our studied population.
In present study 82% children were SFD at the time of birth, while 18% were AFD. Weight for age was <-3SD in 88% children, weight for height was <-3SD in 100% children; while 22.0% had MUAC ≤11.5 cm, 64% had visible wasting, and 10% had pedal edema. Sahoo DP et al15 reported 37.8% of the children were underweight (weight for age) and 14.4% were severely underweight. Stunting (height for age) was present in 37% of the children, and 5.2% were severely stunted. Wasting (weight for age) was present in 35.6% of the children and 14.8% were severely wasted which was similar to the present study. In our study the anthropometric parameters (i.e. W/A, W/H) are more affected as compared to other studies. This could be because of low birth weight, poor socioeconomic status, local beliefs and taboos regarding feeding practices in our studied population.
In our study, 39% of children were hypocalcemic, 16% had low phosphorus levels and 6% had Alkaline e phosphate levels >383U/L. Fifty eight percent of all studied children were having Vitamin D levels<20 ng/ml, out of which 28% children had inadequate and 30% had deficient levels. Prevalence of VDD in malnourished children in study conducted by Mehta S16 was 32%. These findings were similar to those seen in Pakistan (33.6%).17 VDD in children from other countries shows variable prevalence, for instance the prevalence among 12–24 month-olds in China was 65.3%.18 This may be because all other studies had different age groups of children. Our data is comparable to the data from these studies which indicate that VDD is prevalent in SAM children. This could be related to poor nutritional intake, poor sunlight exposure and possibly impaired absorption due of enteric dysfunction or a disease process.
We found that age, previous hospitalization, not giving exclusive breastfeeding, protein calorie deficit and lower socioeconomic status were statistically significant (p<0.05) risk factors associated with vitamin D deficiency in SAM children. There were no such extensive previous studies which showed the association of risk factors in SAM patients having deficiency of vitamin-D. So our study is novel to do the extensive evaluation of association of risk factors in SAM patients having deficiency of vitamin-D.
Nutrition is essential for human development during first five years, it not only affects growth and morbidity, but also determines nutritional status of adolescents and adults. The incidence of SAM was found to be higher in younger children i.e. 74.0% in the children less than 3 years of age. The reason may be the fact that growth and the nutritional needs are maximum in younger age group.7
We found that, the incidence of children under SAM among all hospitalized children was 4.2%. Our findings showed marked increase in prevalence as compared with the study performed by Bhadoria AS et al8 who reported a prevalence of SAM as 2.20%. But prevalence of SAM in our study was lower as compared to national prevalence (7.9%).9 Reason of disparity could be-lower parental education and poor occupation of the head of family predispose a child to SAM. In a similar study from Puducherry by Shewade HD et al10, reported the prevalence of SAM among children from slums in the similar age group (6 months–5 years) as 3.60% and Pravana NK et al11 reported the prevalence of SAM among children under the age of 5 years was 4.14%. So the results of studies done by Shewade HD et al10 and Pravana NK et al11 are comparable with the results of our study.
In the present study, chief complaints of studied children were failure to gain weight in 100%, fever in 74.0%, followed by cough in 42.0%, diarrhea in 18.0%, convulsion in 14.0%, lethargy in 10.0%, pallor in 7%, bleeding manifestations in 2%, generalized body swelling and weight loss in 1.0% each.
Fifty five percent of the studied children were on Mixed (breast+ top) feeding, 40% were on Breast feeding and 5.0% were on top feeding in first 6 months of life. Similar findings were reported by Pravana NK et al11 and Prashanth MR et al12 in their respective studies. This showed that feeding practices are not effective and may be a contributory factor for malnutrition.
All the studied patients were found to be calorie deficient and 95% had protein deficit. Prashanth MR et al12 reported calorie deficit in 79.6% and protein deficit in 66.0% patients. There is considerable uncertainty regarding the estimated calorie and protein intakes of breastfed children, and the interpretation of dietary intakes has to be viewed with caution.
Ninety percent children belonged to upper lower class, followed by lower middle (8.0%) and upper middle (2.0%). Pravana NK et al11 reported the majority of their patients of lower group. Studies conducted by Dwivedi et al13 and Avachat et al14 came up with similar inferences. Better socioeconomic conditions are associated with more spending capacity, better living conditions and better-updated knowledge of the parents, hence could result in reduction of malnutrition.
In our study, 39% of the mothers were educated till high school, 35% till intermediate, followed by 15% upto primary/middle school, 6% were illiterate and 5.0% were graduate. Sahoo DP et al15 reported almost the similar data as in present study. It is the fact that mother’s education is associated with the awareness about the proper child-rearing practices, better health-seeking attitude and better knowledge about feeding and immunization.
We found that, 99.0% of the cases have utilized the services of Anganwadi Centre. This showed the health seeking behavior of the studied population, although there was delay in seeking tertiary health care services. This could be because of poor socioeconomic status, difficult terrain and local beliefs and taboos prevailing in our studied population.
In present study 82% children were SFD at the time of birth, while 18% were AFD. Weight for age was <-3SD in 88% children, weight for height was <-3SD in 100% children; while 22.0% had MUAC ≤11.5 cm, 64% had visible wasting, and 10% had pedal edema. Sahoo DP et al15 reported 37.8% of the children were underweight (weight for age) and 14.4% were severely underweight. Stunting (height for age) was present in 37% of the children, and 5.2% were severely stunted. Wasting (weight for age) was present in 35.6% of the children and 14.8% were severely wasted which was similar to the present study. In our study the anthropometric parameters (i.e. W/A, W/H) are more affected as compared to other studies. This could be because of low birth weight, poor socioeconomic status, local beliefs and taboos regarding feeding practices in our studied population.
In our study, 39% of children were hypocalcemic, 16% had low phosphorus levels and 6% had Alkaline e phosphate levels >383U/L. Fifty eight percent of all studied children were having Vitamin D levels<20 ng/ml, out of which 28% children had inadequate and 30% had deficient levels. Prevalence of VDD in malnourished children in study conducted by Mehta S16 was 32%. These findings were similar to those seen in Pakistan (33.6%).17 VDD in children from other countries shows variable prevalence, for instance the prevalence among 12–24 month-olds in China was 65.3%.18 This may be because all other studies had different age groups of children. Our data is comparable to the data from these studies which indicate that VDD is prevalent in SAM children. This could be related to poor nutritional intake, poor sunlight exposure and possibly impaired absorption due of enteric dysfunction or a disease process.
We found that age, previous hospitalization, not giving exclusive breastfeeding, protein calorie deficit and lower socioeconomic status were statistically significant (p<0.05) risk factors associated with vitamin D deficiency in SAM children. There were no such extensive previous studies which showed the association of risk factors in SAM patients having deficiency of vitamin-D. So our study is novel to do the extensive evaluation of association of risk factors in SAM patients having deficiency of vitamin-D.
Limitations:
Study was conducted in single centre with small sample size. There were confounding factors in the study, those were not analysed like children who were small for gestation infants who can be in there catch growth period, associated comorbid conditions which is not included in exclusion criteria and infants <6 months were also included in the study. Hence multicentric detailed studies with larger sample size are recommended. | | | | Conclusion | | The clinical signs of rickets are unlikely to present in SAM patient and thus vitamin D deficiency is often under diagnosed. On initiation of nutritional rehabilitation the overt signs of rickets develop if vitamin D deficiency is not treated. As per this study, significant percentage (58%) of SAM patients had vitamin D deficiency. Hence, there is a need for active surveillance and management of the same. | | | | Compliance with Ethical Standards | | Funding None | | | | Conflict of Interest None | | |
- Guideline WHO. Updates on the management of severe acute malnutrition in infants and children. Geneva: World Health Organization. 2013; 2013:6-54.
- Ashworth A. Guidelines for the inpatient treatment of severely malnourished children. World Health Organization; 2003.
- Kulkarni B, Mamidi RS. Nutrition rehabilitation of children with severe acute malnutrition: Revisiting studies undertaken by the National Institute of Nutrition. Indian J Med Res 2019; 150:139-52. [CrossRef] [PubMed] [PMC free article]
- Fiscaletti M, Stewart P, Munnns CF. The importance of vitamin D in maternal and child health: a global perspective; Public Health Rev. 2017; (38):19. [CrossRef] [PubMed] [PMC free article]
- Goyal S, Agarwal N. Risk factors for severe acute malnutrition in Central India; Inter J Medical Sci Res and Prac 2015; 2(2): 70-72.
- WHO (2009). Growth Standards and the Identification of Severe Acute Malnutrition in Infants and Children: A Joint Statement by the World Health Organisation and the United Nations Children's Fund Institute of Medicine, Food and Nutrition Board. Dietary Reference Intakes for Calcium and Vitamin D. Washington, DC: National Academy Press, 2010.
- Mehta S. vitamin d levels among children with severe acute malnutrition. World Journal of Pharmaceutical Research. 2017; 6(5):781-785. [CrossRef]
- Bhadoria AS, Kapil U, Bansal R, et al. Prevalence of severe acute malnutrition and associated sociodemographic factors among children aged 6 months-5 years in rural population of Northern India: A population-based survey. J Family Med Prim Care. 2017 Apr-Jun; 6(2): 380-385. [CrossRef] [PubMed] [PMC free article]
- Mumbai: IIPS: 2005-2006; 2007. [Last accessed on 2016 Sep 15]. International Institute for Population Sciences and Macro International National Family Health Survey (NFHS-3).
- Shewade HD, Sunderamurthy B, Jayakumar N, et al. Prevalence of severe acute malnutrition (SAM) among under-five children: A community-based cross-sectional study from Puducherry India. Indian J Matern Child Health. 2013; 15:1-7.
- Pravana NK, Piryani S, Chaurasiya SP, et al. Determinants of severe acute malnutrition among children under 5 years of age in Nepal: a community-based case-control study. BMJ Open. 2017;7(8): e017084. [CrossRef] [PubMed] [PMC free article]
- Prashanth MR, Savitha MR, Prashantha B. Risk factors for severe acute malnutrition in under- five children attending nutritional rehabilitation center of tertiary teaching hospital in Karnataka: a case control study. Int J ContempPediatr.2017;4(5):1721-26. [CrossRef]
- Dwivedi SN, Banerjee N, Yadav OP. Malnutrition among children in an urban Indian slum and its associations. Indian J Matern Child Health 1992; 3:79-81.
- Avachat SS, Phalke VD, Phalke DB, et al. A cross-sectional study of socio- demographic determinants of recurrent diarrhoea among children under five of rural area of Western Maharashtra, India. Australas Med J 2011; 4:72-5. [CrossRef] [PubMed] [PMC free article]
- Sahoo DP, Dehmubed A, Jajulwar MB. An epidemiological study of acute malnutrition in children of age 6 months to 5 years in an Urban Slum of Mumbai, Maharashtra. J Datta Meghe Inst Med Sci Univ 2017; 12:181-6. [CrossRef]
- Mehta S. vitamin d levels among children with severe acute malnutrition. World Journal of Pharmaceutical Research. 2017; 6(5):781-785. [CrossRef]
- Ejaz MS, Latif N. Stunting and micronutrient deficiencies in malnourished children. J Pak Med Assoc 2010; 60: 543-7.
- Strand MA, Perry J, Jin M, et al. Diagnosis of rickets and reassessment of prevalence among rural children in northern China. Pediatr Int 2007; 49: 202-9. [CrossRef] [PubMed]
DOI: https://doi.org/10.7199/ped.oncall.2025.21
|
| Cite this article as: | | Tulsi N, Sharma S, Rehalia N, Sharma M. Status of Vitamin D Levels and Associated Risk Factors in Severe Acute Malnutrition in Children Up To 60 Months Of Age- A Cross Sectional Study From North-West India. Pediatr Oncall J. 2025;22: 57-63. doi: 10.7199/ped.oncall.2025.21 |
|