Shalini Avasthi1, Sunil Taneja2, Devendra Agrawal3.
1Consultant paediatrician, UHM, Hospital, Kanpur,
2Consultant paediatrician, Madhuraj Hospital, Kanpur,
3Pediatric Surgeon, Madhuraj Hospital, Kanpur.
ADDRESS FOR CORRESPONDENCE
Dr Shalini Avasthi, L-30 GSVM campus, Swaroop Nagar, Kanpur, India.
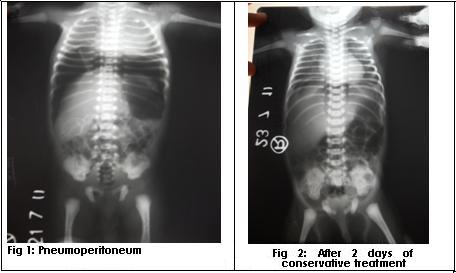
Email: shalini.avasthi@rediffmail.com | | Keywords | | Pneumoperitoneum; necrotizing enterocolitis; pneumothorax, pneumomediastinum | | | A new born, 34 week by gestation, a product of in vitro fertilization was admitted to the NICU with complaints of respiratory distress on first day of life. Baby was delivered by lower segment caesarean section (LSCS), cried soon after birth. There was no history of leaking per vaginum prior to the birth of the baby. The chest x-ray showed mild perihilar infiltrates bilaterally. After sending the sepsis screen and blood culture, injectable antibiotics were started. He was given oxygen by head box at the flow rate of 2 litres per minute. On day third the child gradually improved with decreased respiratory rate and was maintaining saturation without oxygen. On the same day, the child suddenly developed abdominal distension with bilateral scrotal oedema. On examination child was active, capillary refill time was less than 2 seconds, peripheral pulses were palpable. Abdomen was distended but soft. There was no tenderness, no visible peristalsis, bowel sounds were normal and there was bilateral inguinal hernia was present. Serum electrolytes were normal. Abdominal x-ray erect showed free gas under both domes of diaphragm (fig: 1). There was no evidence of pneumothorax, bilateral lung fields were clear. Ultrasound showed normal domes of diaphragm, no air in pleural cavity and air under both domes of diaphragm. As there were no features of air in the pleural cavity, no clinical features of necrotizing enterocolitis (NEC) and neither there was any antecedent event like instrumentation or abdominal surgery, which can lead to gastrointestinal perforations, the diagnosis of benign pneumoperitoneum was made and we planned to manage the baby conservatively. He was kept fasting with elevated head end, abdominal girth monitoring and repeated tube suction. A laprotomy was planned if air in the repeated x-rays increased or distension increased. Gradually the distension reduced, stool passed normally and the repeat x-ray after 48 hours was normal (figure: 2). Oxygen was stopped, tube feeding was started and increased gradually and the neonate was on full feeds on day fourteen of life and discharged.
Pneumoperitoneum in the newborn most commonly arises from a perforated hollow viscus. (1) Also it is associated with pulmonary air leak syndromes- pneumothorax, pneumomediastinum in neonates on mechanical ventilation. (2) Pneumoperitoneum without viscus rupture is rare at any pediatric age. Koklu et al reported a neonate of 34 week gestation with hyaline membrane disease. The baby was treated with surfactant, mechanical ventilation, improved, extubated and when he was about to be discharged developed sudden onset isolated pneumoperitoneum without any cause. (3) Shah et al reported a 36 week gestation male child who presented with abdominal distention with any other complaint on eight day of life. He had pneumoperitoneum without any intrathoracic pathology. (4) Vohra et al described a case of pneumoperitoneum a newborn who had no evidence of an associated pulmonary air leak or bowel perforation. Pathologic examination of the placenta showed associated acute chorioamnionitis and funisitis. (5) Khan et al retrospectively analyzed 89 neonates admitted with a diagnosis of pneumoperitoneum during the period of 3 years. NEC remained the single major cause of pneumoperitoneum in the newborn; however, in 44 (49.4%) patients the cause was not related to NEC. Perforated pouch colon, isolated colonic perforations, caecal perforations, gastric and duodenal perforations were the main causes of pneumoperitoneum not related to NEC. There were seven patients in whom no cause of pneumoperitoneum could be ascertained. (6)
We present this case because at the time of diagnosis of pneumoperitoneum the patient was breathing spontaneously. Also there was no evidence of air leak. In the present case the paediatric surgeon decided not to go for an unnecessary laprotomy and baby was managed conservatively, improved, led us to believe that there was no associated viscus rupture. Authors conclude that every case of neonatal pneumoperitoneum management needs individualised approach, we should not be impatient for doing the exploratory laprotomy.
Competing interests: none
Funding: none | | | | Compliance with Ethical Standards | | Funding None | | | | Conflict of Interest None | | |
- Zerella JT, McCullough JY. Pneumoperitoneum in infants without gastrointestinal perforation. Surgery. 1981; 89: 163-167. [PubMed]
- Knight PJ, Abdenour G. Pneumoperitoneum in the ventilated neonate: respiratory or gastrointestinal origin? J Pediatr. 1981; 98: 972-974. [CrossRef]
- Koklu E, Akcakus M, Turan C, Altunay L, Canpolat M. Benign pneumoperitoneum in a newborn: a case report. Erciyes Med J 2007; 29: 245-247.
- Shah RS, Patel MP, Pikale HS, Kulkarni BK, Borwankar SS. Benign neonatal pneumoperitoneum--an enigma. J Postgrad Med. 1992; 38: 84-85. [PubMed]
- Vohra K, Jenkins K, Klotz DH, French JH. Neonatal pneumoperitoneum of uncertain etiology. J Natl Med Assoc. 1992; 84: 633-635. [PubMed] [PMC free article]
- Khan TR, Rawat JD, Ahmed I, Rashid KA, Maletha M, Wakhlu A, et al. Neonatal pneumoperitoneum: a critical appraisal of its causes and subsequent management from a developing country. Pediatr Surg Int. 2009; 25: 1093-1097. [CrossRef]
DOI: https://doi.org/10.7199/ped.oncall.2012.4
|
| Cite this article as: | | Agrawal D, Taneja S, Avasthi S. SPONTANEOUS IDIOPATHIC PNEUMOPERITONEUM IN A NEWBORN. Pediatr Oncall J. 2012;9: 16-17. doi: 10.7199/ped.oncall.2012.4 |
|