Poovazhagi Varadharajan, Nisha Bashyam, Srinithi Kannan, Seenivasan Subramani, Ramesh Subramanian.
Paediatric Intensive Care Unit, Institute of Child Health and Hospital for Children, Chennai, Tamil Nadu, India.
ADDRESS FOR CORRESPONDENCE
Poovazhagi Varadharajan, 19 & 20, Aandal Garden, Ramapuram, Chennai - 600089.
Email: poomuthu@gmail.com | | Abstract | | A 12 years female with history of fever, abdomen pain, vomiting and loose stools for 4 days, presented to emergency room with hypotensive shock. Resuscitated with normal saline bolus, inotropes, intubated and shifted to paediatric intensive care unit [PICU]. Echo revealed LV dysfunction and small aneurysm of right coronary artery. Diagnosed as multisystem inflammatory syndrome [MIS-C] and received intravenous immunoglobulin, injection methylprednisolone and aspirin. Serial echo revealed thrombi in left ventricle along the apex and interventricular septum. She developed right hemiparesis during the hospital stay. Neuroimaging revealed left middle cerebral artery infarct. She was on heparin infusion. Child later developed intracranial bleed with haemorrhagic transformation of the infarct during the hospital stay with raised intracranial pressure and refractory seizures. She was IgG covid antibody reactive. Despite the best of efforts, the child died in hospital. A rare presentation of intracardiac thrombi in multisystem inflammatory syndrome in children [MIS-C]. | | | | Keywords | | MIS-C, Intracardiac thrombi, LV dysfunction. | | | | Case Report | A 12 years female was brought with fever for 4 days, pain abdomen, vomiting and loose stools to the emergency department. Her airway was stable, respiratory rate was 36/min, heart rate was 140/min, peripheral pulses were feeble, blood pressure was 60/40 mmHg. She had bilateral conjunctival congestion and right subconjunctival bleed. She was resuscitated with 60 ml/kg of normal saline bolus, intubated and started on epinephrine infusion at 0.1 mic/kg/mt and shifted to PICU.
Laboratory parameters are summarized in Table 1. Complete blood count revealed neutrophilic leukocytosis with lymphopenia. Prothrombin time was 19 sec, activated partial thromboplastin time was 35.63 sec and International Normalised Ratio was 1.5. Initial ECHO showed mild LV dysfunction with ejection fraction of 41% and minimal pericardial effusion. Right coronary artery showed an aneurysm with a Z score of +2.54 and other coronaries were normal. Her inflammatory markers were elevated with D-dimer of 6.65 μg/ml (Reference range < 0.46 µg/ml) and IgG covid antibody was positive with a titre of 83.77 AU/ml (Reference range < 10 AU/ml). She was covid RT PCR negative. With a possible diagnosis of MIS-C she was started on intravenous immunoglobulin at 2 g/kg and methylprednisolone at 10 mg/kg/day. Serial echo revealed fall in EF with lowest value of 33% [Table 2] and thrombi at the left ventricular apex and interventricular septum as shown in Figure 1. In view of right fundal bleeds aspirin and heparin were withheld. Neuroimaging revealed infarct over the left frontoparietal region [Figure 2]. Child had persistent fever spikes and fall in hemoglobin and platelet counts. Bone marrow aspiration showed hemophagocytic lymphohistiocytosis. Fever work up including blood culture, urine culture, enteric fever, dengue, leptospirosis and scrub serology were negative.
Figure 1. ECHO showing Left ventricle thrombus along Interventricular septum.
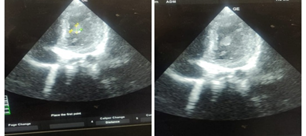
Figure 2. CT Brain showing infarct involving left frontoparietal region on Day 14.
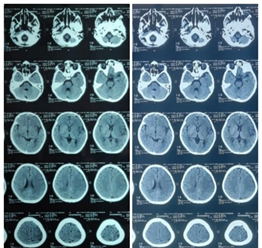
Table 1. Summary of laboratory parameters.
| Day of stay |
1 |
3 |
6 |
10 |
| Total count (cells/cu.mm) (4500 – 13000) |
21400 |
18800 |
11000 |
6000 |
| Hemoglobin (g/L) (12.2 – 14.2) |
9.2 |
9.8 |
8.2 |
7.2 |
| Differential count (PMN/Lymph/Eosi) (54/38/6) |
90.7/4.3/5 |
60.6/23.5/15.7 |
78.3/19.7/2 |
83/15.6/1.4 |
| ESR mm/hr (<20) |
44 |
39 |
|
90 |
| CRP mg/dl (<6 mg/dl) |
6 |
24 |
89 |
51.9 |
| Platelet (lakhs/cu.mm) (1.5 – 4.5) |
2.77 |
1.63 |
1.46 |
1.29 |
| Urea/creatinine (mg/dl) (<40 / 0.5 – 1.0) |
66/1.7 |
89/0.9 |
80/0.9 |
67/0.7 |
| SGOT/PT (U/L) ( <46 / <35) |
69/71 |
64/52 |
55/44 |
106/65 |
| CXR |
Normal |
|
Normal |
|
| Ferritin (ng/ml) (<300) |
|
454 |
|
1456 |
| LDH (U/L) (120 – 330) |
|
622 |
|
|
| Covid RT PCR |
Negative |
|
|
|
| IgG covid antibody (AU/ml) |
83.77 |
|
|
|
| D dimer (µg/ml) (<0.46) |
6.65 |
|
|
|
| ANA/dsDNA |
Negative |
|
|
|
Table 2. Echo findings.
| Day of stay |
1 |
4 |
7 |
10 |
15 |
27 |
| Ejection fraction |
41% |
33% |
48% |
59.6% |
58% |
60% |
Coronary (Z score)
RCA*
LMCA*
LAD*
|
+2.54 |
+2.54
+0.80
+0.62 |
|
+2.54
+0.76
+0.64 |
-0.44
-0.49
-1.27 |
|
| Other Findings |
pericardial effusion |
|
|
Thrombi
(2 x 1.5 cm)
(0.5x1.1 cm) |
Thrombi
(0.5x 0.5 cm) |
No clots |
*RCA - Right Coronary Artery; LMCA - Left Main Coronary Artery; LAD – Left Anterior Descending Artery.
Management and outcome:
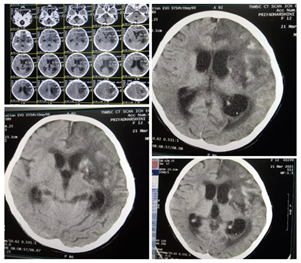
Unfractionated heparin was given at a bolus of 75 U/Kg bolus followed by 20 U/Kg/hr infusion. Child required inotropes for 13 days. On day 14, child developed right hemiparesis and CT brain revealed infarct involving left frontoparietal region [Figure 2]. She was extubated on day 20. MR angiogram revealed left MCA infarct. On day 21, oral nicoumalone at a dose of 0.2 mg/kg was started in addition to heparin under PT and aPTT monitoring. heparin was stopped on day 24. Nicoumalome and aspirin were continued. Repeat ECHO on day 27, showed no evidence of thrombi and ejection fraction was 60%. Protein C, S, Antithrombin III were normal. β2 glycoprotein [IgG & IgM] were negative. On day 37, anticoagulants were stopped as INR was prolonged. Subsequently, during hospital stay she developed malena and refractory hypotensive shock and seizures. She was reintubated. Repeat CT Brain showed subacute infarct of left frontoparietal region with hemorrhagic transformation [Figure 3]. Despite all efforts, child could not be saved.
Figure 3. CT brain revealing subacute hemorrhagic transformation of infarct of left frontoparietal region on Day 38.
| | | | Discussion | Initial presentation with acute febrile illness, GI symptoms and hypotensive shock with elevated inflammatory markers and covid antibodies favoured a diagnosis of MIS-C. Isolated prothrombotic event is unlikely to present with LV dysfunction and hypotensive shock. Reported cardiac manifestations1,2 in MIS-C includes cardiogenic shock, cardiac arrhythmias, pericardial effusion and coronary artery dilation.
SARS-CoV-2 generates a prothrombotic state with pulmonary embolism being the most common thrombotic manifestation and incidence of arterial thrombi appears to be rare. Elevated D-dimer may be an independent risk factor for predicting poor outcome. The proposed mechanisms leading to this hypercoagulable state are localized intravascular coagulopathy, excessive inflammatory cytokines, endothelial dysfunction, activation of monocytes-macrophages, abundant activation of neutrophils leading to neutrophil extracellular traps, activation of dysregulated complement system and renin angiotensin system with initial inciting event igniting the cycle of thrombosis at pulmonary alveoli.3
Covid-19 induced inflammation is an important factor for cardiac complications. IL 6 and other cytokines inhibit the natural inhibitors of hemostasis and cause thrombosis. Endothelial injury by covid-19 infection adds to the thrombotic formation. Intracardiac thrombus has been rarely reported in MIS-C4,5,6 with a reported mortality of 39%. Majority of the cases resolve with medical therapy alone and only few require surgical thrombectomy. Perhaps, this is probably one of the rare reports of intracardiac thrombi as a manifestation of MIS-C among Indian children, in this covid pandemic.
| | | | Compliance with Ethical Standards | | Funding None | | | | Conflict of Interest None | | |
- Sperotto F, Friedman KG, Son MB, VanderPluym CJ, Newburger JW, Dionne A. Cardiac manifestations in SARS-CoV-2-associated multisystem inflammatory syndrome in children: a comprehensive review and proposed clinical approach. European journal of pediatrics. Springer; 2021 Feb;180:307-22. [CrossRef] [PubMed] [PMC free article]
- Basu-Ray I, Adeboye A, Soos MP, Almaddah NK. Cardiac manifestations of coronavirus (COVID-19). InStatPearls[Internet]. StatPearls Publishing; 2022 Jan 15.
- Abou-Ismail MY, Diamond A, Kapoor S, Arafah Y, Nayak L. The hypercoagulable state in COVID-19: Incidence, pathophysiology, and management. Thrombosis research. Elsevier; 2020 Oct 1;194:101-15. [CrossRef] [PubMed] [PMC free article]
- John JB, Cron SG, Kung GC, Mott AR. Intracardiac thrombi in pediatric patients: presentation profiles and clinical outcomes. Pediatric Cardiology. Springer; 2007 Jun;28:213-20. [CrossRef] [PubMed]
- Bigdelian H, Sedighi M, Sabri MR, Dehghan B, Mahdavi C, Ahmadi A, et al. Case report: Acute intracardiac thrombosis in children with Coronavirus Disease 2019 (COVID-19). Frontiers in Pediatrics. 2021 Jun 25;9:656720. [CrossRef] [PubMed] [PMC free article]
- Schroder J, Lund MA, Vejlstrup N, Juul K, Nygaard U. Left ventricular thrombus in multisystem Inflammatory syndrome in children associated with COVID-19. Cardiology in the Young. Cambridge.org; 2022 Jan; 32(1): 138-41. [CrossRef] [PubMed] [PMC free article]
DOI: https://doi.org/10.7199/ped.oncall.2023.39
|
| Cite this article as: | | Bashyam N, Varadharajan P, Kannan S, Subramani S, Subramanian R. Intracardiac thrombi in Multisystem inflammatory syndrome in children. Pediatr Oncall J. 2023;20: 95-97. doi: 10.7199/ped.oncall.2023.39 |
|