Ana Gisela Oliveira1, Carolina Figueiredo2, Helena Torrão3, Sílvia Ferreira Silva4.
1Serviço de Pediatria, Centro Hospitalar Tondela-Viseu, EPE, Viseu, Portugal,
2Serviço de Pediatria, Hospital Divino Espírito Santo de Ponta Delgada, Ponta Delgada, Portugal,
3Serviço de Radio-oncologia, Instituto Português de Oncologia do Porto, EPE, Porto, Portugal,
4Serviço de Oncologia Pediátrica, Instituto Português de Oncologia do Porto, EPE, Porto, Portugal.
ADDRESS FOR CORRESPONDENCE
Ana Gisela Oliveira, Rua do Mar, nº 871, 4405-760, Madalena, Vila Nova de Gaia.
Email: a27135@fcsaude.ubi.pt | | Abstract | Twelve-years-old girl, with prenatal diagnosis of right renal agenesis, menarche at eleven-years-old, presenting with dysmenorrhea, metrorrhagia and menorrhagia.
On objective examination, she presented diffuse pain on deep abdominal palpation, without masses. Laboratory tests were unremarkable. A supra-pubic pelvic ultrasound revealed a heterogeneous nodular structure with benign characteristics measuring 4x3,5cm, which seemed to correspond to a teratoma.
The patient was referred to pediatric oncology. The analytical study was extended, including tumor markers, without alterations. Abdominal-pelvic CT and MR scan revealed uterine malformation and distension of the vaginal canal by hematic content.
Diagnosis of Herlyn-Werner-Wunderlich Syndrome (HWWS) was made.
Oriented to gynecology and submitted to drainage of the hematocolpos. Currently, she is on oral iron, due to anemia, contraceptives and analgesia with progressive improvement.
HWWS is a rare congenital anomaly of the female urogenital tract, characterized by bicorporeal uterus, obstructed hemivagina and ipsilateral renal agenesis. Symptoms are usually after menarche and nonspecific. | | | | Keywords | | urogenital abnormalities; mullerian ducts; mesonephric ducts; hematocolpos; Herlyn-Werner-Wunderlich syndrome. | | | | Case Report | We discuss the case of a 12-year-old girl who was prenatally diagnosed with right renal agenesis and hypertension and who developed incapacitating dysmenorrhea, metrorrhagia and menorrhagia within three months of her condition evolving. The patient additionally described sporadic abdominal pain that wasn't necessarily related to her menstrual irregularities. She reached menarche at the age of eleven and currently has not initiated sexual activity.
Regarding any pertinent family medical history, the patient had a paternal aunt who had breast cancer and a paternal grandmother who had been diagnosed with an ovarian tumor.
She displayed generalized pain on deep abdominal palpation during an objective examination, but there were no palpable lumps or indications of peritoneal irritation. There were no additional details discovered.
The results of the lab tests were ordinary. An ultrasound of the suprapubic pelvis located a uterus with normal biometry and texture. The right ovary's pubertal morphology was typical. Unidentified was the left ovary. With internal echoes measuring 4x3,5 cm, a swollen structure right posterior to the bladder was seen in the midline. It was interpreted as potentially being a teratoma.
Given its oncological suspicion, the patient was referred from general pediatric consultation, where she was previously followed up due to renal agenesis, to a pediatric oncology center.
In addition, the analytical analysis was extended and indicated no abnormalities, including negative tumor markers (alpha-fetoprotein, beta human chorionic gonadotropin and cancer antigen 125). The right kidney was absent, there were no obvious masses, the uterus was lateralized to the right and showed indentation of the fundal contour, corresponding to uterine malformation and the vaginal canal was enlarged by hypodense and heterogeneous material (Figure 1).
Figure 1 (a). Axial and sagital CT demonstrating right renal agenesis.
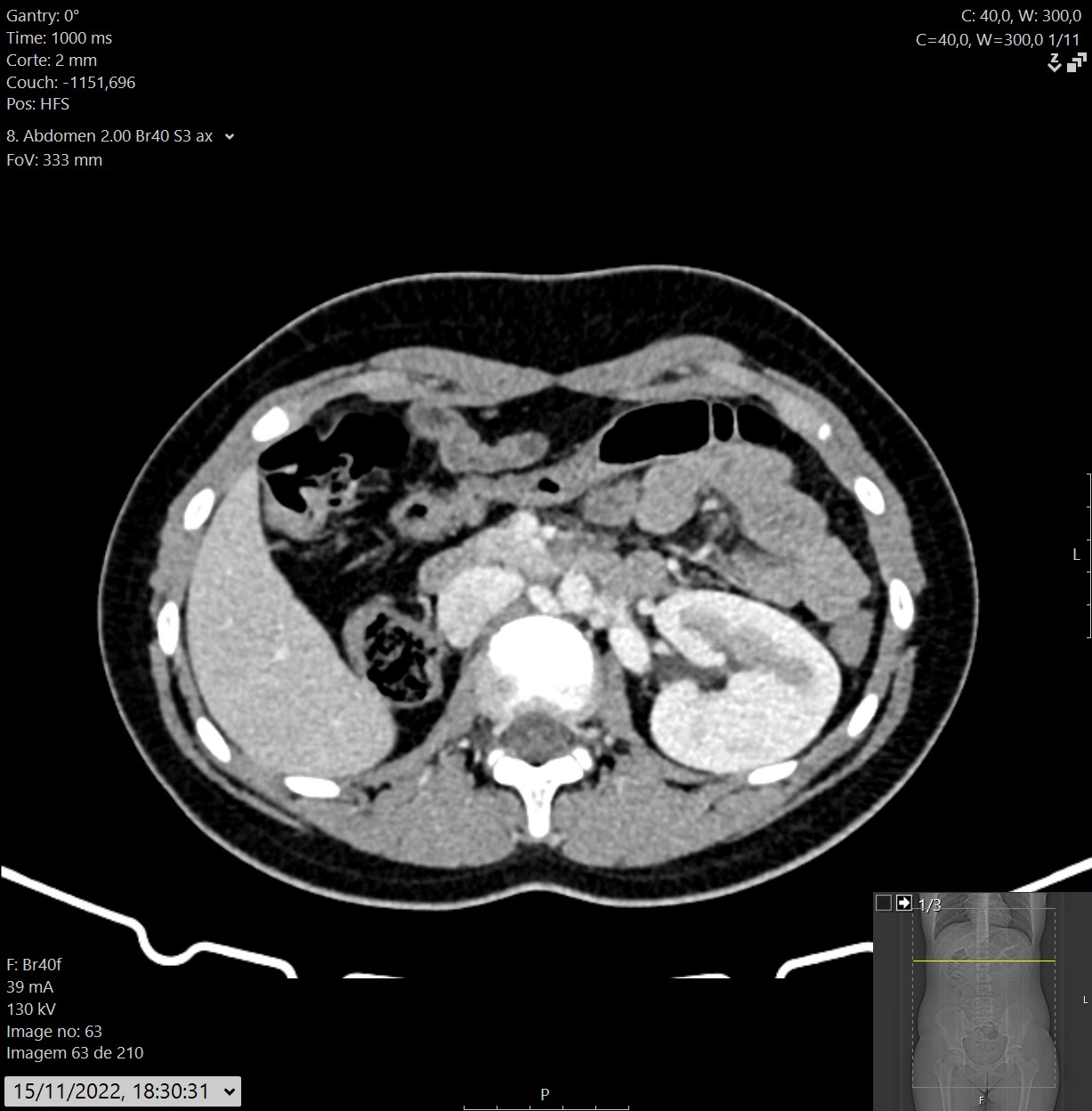
Figure 1 (b). distendend vaginal lumen.
Given the clinical history and suggestive TC scan images, Herlyn-Werner-Wunderlich Syndrome (HWWS) diagnosis was suspected.
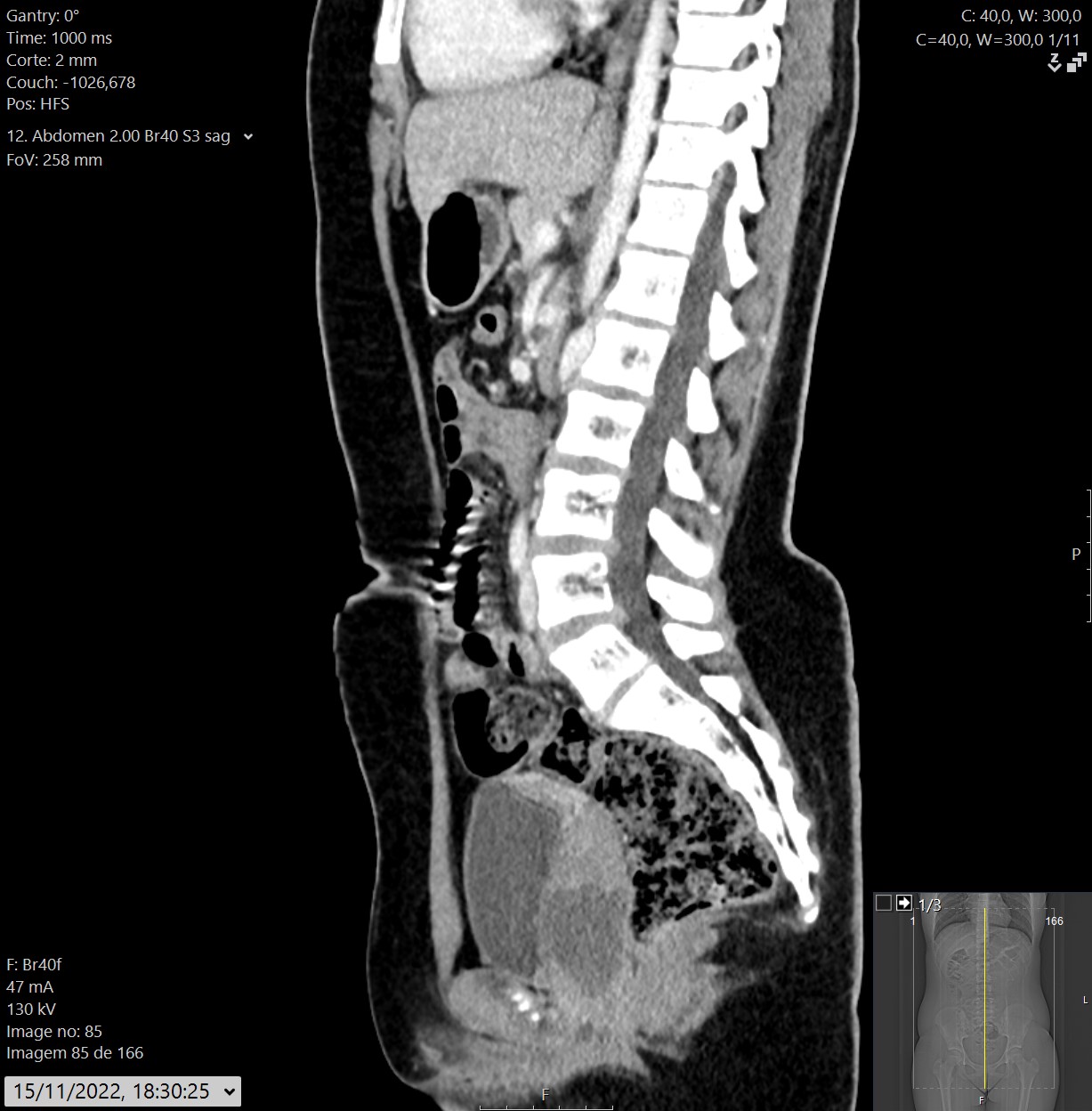
In this context, for better characterization pelvic MRI was performed, demonstrating a bicorporeal uterus with a double cervix normally formed in the right lateral deviation, two hemi-vaginas (U3bC2V2, according to the ESHRE/ESGE classification), the right one filled with hematic content, compatible with hematocolpos (Figure 2). The prenatal diagnosis of right renal agenesis was corroborated (Figure 3). The findings framed the HWW syndrome.
The patient had septostomy-assisted hematocolpos drainage after being sent to gynecology at a hospital in a residential area. The patient is currently taking oral iron for anemia, which was discovered in a recent complete blood count. She also started using oral contraceptives and began taking paracetamol and ibuprofen for pain relief and her condition has improved over time.
Figure 2 (a). Image of abdominal - pelvic magnetic resonance imaging sagittal T2-weighted study showing hematocolpos.

Figure 2 (b). Image of abdominal - pelvic magnetic resonance imaging axial T2-weighted study showing bicorporeal uterus.
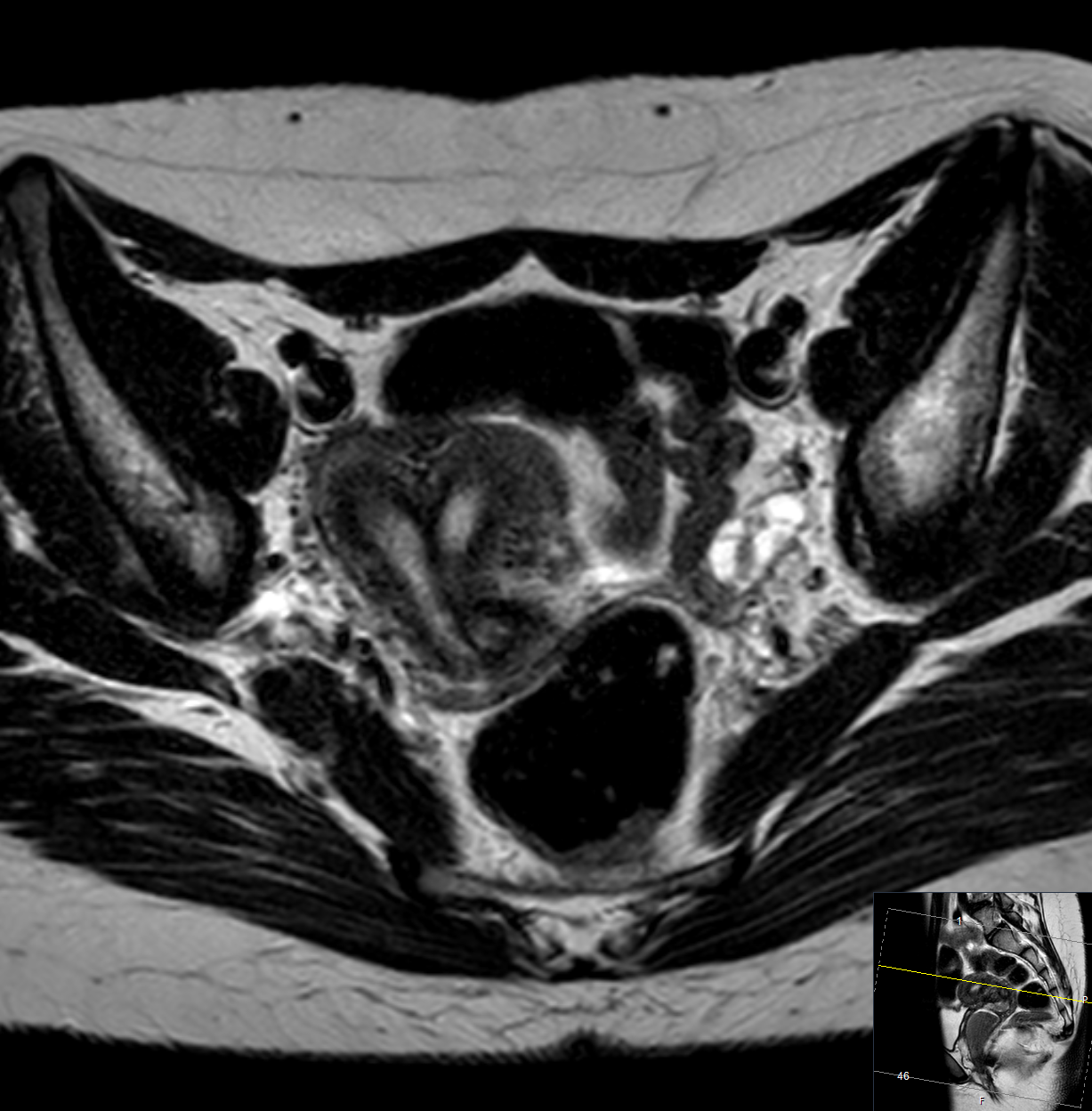
Figure 3. Abdominal- pelvic MR showing right renal agenesis. It is possible do define two vaginal lumens, the most cranial distended with heterogeneous content.

| | | | Discussion | HWWS is a Mullerian and Wollf duct-involved congenital abnormality of the urogenital tract with a reported prevalence of 2%-3% and a frequency of 1 in 200-1 in 600 among fertile women.1 Although the exact process is unknown, its etiology is connected to the aberrant development of these two embryonic tissues.2 In more than half of patients, renal agenesis is indicative of an ipsilateral obstructive Mullerian abnormality. The right side predominates in these anomalies, occurring twice as frequently as the left side.3
HWWS is characterized by the triad of ipsilateral renal agenesis, blocked hemivagina and bicorporeal uterus. It can be categorized according to whether the hemivagina is entirely or partially blocked, hence the clinical presentation may change depending on when the diagnosis was made.1,2,3 When the blockage is only partially present, the first symptoms typically arise 6 to 9 months following menarche because one hemivagina externalizes its menstrual flow while the second, obstructed hemivagina gradually develops a hematocolpos.3 However, a delayed diagnosis could be brought on by a delayed presentation with vague and fluctuating symptoms.4 Pain, dysmenorrhea and an abdominal mass in the lower abdomen as a result of hematocolpos and/or hematometra are the most typical symptoms.5
Physical examination typically reveals a unilateral pelvic mass, more commonly on the right than the left, with a ratio of 2:1.1
Due to the rarity of the illness, the diagnosis is frequently challenging, necessitating a high index of suspicion. The imaging differential may include an adnexal mass such as a teratoma, cystadenoma, or endometrioma, as was the case in the current instance when uterovaginal restriction causes considerable dilatation. Since MRI is the gold standard for diagnosis, it assesses the morphology of the uterus, cervix and vagina, as well as the degree of blockage and fluid contents. MRI can simultaneously identify problems such as endometriosis and identify related renal agenesis.5 However, given the simpler access, the most popular initial investigations are abdominal and pelvic US and CT.4
Surgery is the only option for treatment. If a hematocolpos is present, it must be immediately excised and drained to relieve the obstruction. A septoplasty is then performed to completely remove the septum that separates the two hemivaginas.3 Pyohematocolpos or pyosalpinx are possible side effects of this illness and may result in pelvic peritonitis. Infertility and endometriosis are long-term consequences.6,7
Given the embryologic connection between urological and gynecological malformations, a gynecological imaging scan should be carried out when a prenatal diagnosis of unilateral renal agenesis in newborn females is known to rule out uterine and vaginal abnormalities.3
A high index of suspicion in patients with renal anomalies and endometriosis is needed to detect the Herlyn-Werner-Wunderlich syndrome for timely diagnosis to avoid complications from the syndrome.6,7
| | | | Compliance with Ethical Standards | | Funding None | | | | Conflict of Interest None | | |
- Li, X., Liu, T., & Li, L. Herlyn-Werner-Wunderlich syndrome and its complications: A report of two cases and literature review. Radiology Case Reports, 2021;16(8), 2319-2324. Published 2021 Jun 21. doi:10.1016/j.radcr.2021.05.055. [CrossRef] [PubMed] [PMC free article]
- Panaitescu AM, Peltecu G, Gică N. Herlyn-Werner-Wunderlich Syndrome: Case Report and Review of the Literature. Diagnostics (Basel). 2022;12(10):2466. Published 2022 Oct 12. doi:10.3390/diagnostics12102466. [CrossRef] [PubMed] [PMC free article]
- Horst W, de Melo RC, Theilacker G, Schmitt B. Herlyn-Werner-Wunderlich syndrome: clinical considerations and management. BMJ Case Rep. 2021;14(3):e239160. Published 2021 Mar 4. doi:10.1136/bcr-2020-239160. [CrossRef] [PubMed] [PMC free article]
- Khaladkar SM, Kamal V, Kamal A, Kondapavuluri SK. The Herlyn-Werner-Wunderlich Syndrome - A Case Report with Radiological Review. Pol J Radiol. 2016;81:395-400. Published 2016 Aug 24. doi:10.12659/PJR.897228. [CrossRef] [PubMed] [PMC free article]
- Vo Nhu Q, Le Trong B, Nguyen Thanh T. Herlyn-Werner-Wunderlich syndrome: A report of three cases in adolescents and adult women. Radiol Case Rep. 2021;16(9):2792-2798. Published 2021 Jul 23. doi:10.1016/j.radcr.2021.06.081. [CrossRef] [PubMed] [PMC free article]
- Stanislavsky A, El-Feky M, Vlašiček I, et al. Herlyn-Werner-Wunderlich syndrome. Reference article, Radiopaedia.org (Accessed on 21 Apr 2023, Last revised by Mostafa El-Feky on 15 Mar 2023). doi:10.53347/rID-13877. [CrossRef]
- Alzaiem M, Alatili AA, Alawi A, Zaiem F (2019) Herlyn-Werner-Wunderlich Syndrome: A Rare Cause of Acute Abdomen in Adolescent Girls. Obstet Gynecol Cases Rev 6:156. doi.org/10.23937/2377-9004/1410156. [CrossRef]
DOI: https://doi.org/10.7199/ped.oncall.2024.50
|
| Cite this article as: | | Oliveira A G, Figueiredo C, Torrão H, Silva S F. When the cause is not oncological - a case report of Herlyn-Werner-Wunderlich Syndrome.. Pediatr Oncall J. 2024;21: 110-112. doi: 10.7199/ped.oncall.2024.50 |
|