Anirudh Ghai, Nitika Agrawal, Sandeep Rawal.
Department of Pediatrics, Jaipur Golden Hospital, Delhi, India.
ADDRESS FOR CORRESPONDENCE
Dr Nikita Agrawal, Critical Care Assistant, Pediatric Intensive Care, Department of Pediatrics, Jaipur Golden Hospital, Rohini. Delhi-85, India.
Email: drnitika80@rediffmail.com | A 6 years old male child weighing 52 kg (BMI: 34kg/m2), presented with increased sleepiness and lethargy for 2 days. Patient had similar episodes thrice since 4 years of age for which he was managed with oxygen and antibiotics. He had developmental delay, central hypogonadism and micropenis. Bilateral orchidopexy was done at age of 2 years and he was on thyroid hormone supplement since last 3 years. At admission, patient was drowsy with tachypnea (respiratory rate 36/min). Chest auscultation revealed mild basal crepts with limited chest excursion. Investigations revealed normal hemogram and biochemical reports with arterial blood gas (ABG) showing respiratory acidosis (pH 7.257, pCO2- 96.2mmHg, pO2- 23.5mmHg, HCO3- 41.9mmol/l). Chest X-ray revealed infiltrates in right upper zone and bilateral lower zone with normal cardiac size. In view of hypercapnea, nasopharyngeal synchronized intermittent mechanical ventilation (SIMV) support was started as endotracheal intubation was not feasible due to inadequate direct visual access of glottis. Echocardiography revealed dilated right atrium and ventricle with moderate tricuspid regurgitation and severe pulmonary artery hypertension (PAH) of 64mmHg. Polysomnography study with continuous positive airway pressure (CPAP) titration revealed obstructive sleep apnea and apnea-hypopnea index (AHI) of 15.2. (Figure 1 & Table 1) His lipid profile, renal function tests, thyroid profile, cortisol and growth hormone levels and karyotype were normal. Florescent in situ hybridization (FISH) analysis revealed SNRPN mutation confirming diagnosis of Prader Willi Syndrome (PWS). He was supported with broad spectrum antibiotic, diuretics and sildenafil. He improved clinically and ABG on day2 showed pH 7.46, pCO2-51mm hg, pO2- 77mmhg, HCO3- 36.3 mmol/l. He was gradually weaned to intermittent BiPAP and discharged on domiciliary nocturnal BiPAP, sildenafil and spironolactone along with hypocaloric diet and weight reduction advise. Child was advised close follow up but defaulted and stopped sildenafil as well as BiPAP after about 1year. Further after 4 months, he again came with similar complaints, although pulmonary artery tension was not so high (39mm of Hg). He was again managed with non invasive positive pressure ventilation. Further counseling regarding diet, exercise and domiciliary BiPAP was reinforced and he was discharged.
Fig: 1 Polysomnography showing effect of CPAP on night hypnogram
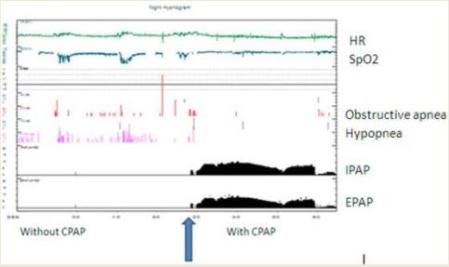
Table 1: Comparison of respiratory events before and after CPAP
| Parameters | Before CPAP | After CPAP | | Central apnea episodes | 1 | 1 | | Obstructive apnea episodes | 24 | 10 | | Mixed apnea episodes | 1 | 3 | | Hypopnea episodes | 76 | 1 | | Maximum duration of apnea (sec) | 126 | 35 | | Apnea index (apnea/hour of TST) | 6.1 | 3.9 | | Hypopnea index (apnea/hour of TST) | 17.8 | 0.3 |
Sleep related breathing disorders (SRBD) and hypercapnea are common in PWS. (1) Ventilatory problems are frequent in PWS cases and the etiology is multifactorial including musculature weakness and morbid obesity, hypothalamic dysfunction and unresponsive chemoreceptors. (1) Various modalities including growth hormone therapy, tracheostomy as well as intermittent positive pressure respiratory support has been tried to improve their ventilation with variable results. (2-4) The nocturnal/ intermittent positive pressure respiratory support has been found to be beneficial in term of improving sleep quality, AHI as well as chemoresponsiveness. As these cases are with mixed central and obstructive component of hypoventilation, a BiPAP support is preferred as was done in our case. (4) Pulmonary artery hypertension and cor pulmonale can occur in these patients and are major causes of mortality in them. Like other naive pulmonary hypertension cases, our patient also responded well to sildenafil treatment. (5) With no separate guideline of treatment duration with sildenafil in PWS, a low dose prolonged treatment with frequent monitoring seems promising. | | | | Compliance with Ethical Standards | | Funding None | | | | Conflict of Interest None | | |
- Jin DK. Systematic review of the clinical and genetic aspects of Prader-Willi syndrome. Korean J Pediatr 2011; 54: 55-63. [CrossRef] [PubMed] [PMC free article]
- Guilleminault C, Cummiskey J. Progressive improvement of apnea index and ventilatory response to CO2 after tracheostomy in improvement of obstructive sleep apnea syndrome. Am Rev Respir Dis 1982; 126: 14- 20. [PubMed]
- Nixon GM, Rodda CP, Davey MJ. Longitudinal Association between Growth Hormone Therapy and Obstructive Sleep Apnea in a Child with Prader-Willi Syndrome. J Clin Endocrinol Metab 2011; 96: 29-33. [CrossRef] [PubMed]
- Wallis C, Stafler P. Managing respiratory problems in Prader-Willi syndrome. Paediatr and Child Health. 2009; 19: 335-337. [CrossRef]
- Humpl T, Reyes JT, Holtby H, Stephens D, Adatia I. Beneficial Effect of Oral Sildenafil Therapy on Childhood Pulmonary Arterial Hypertension: Twelve-Month Clinical Trial of a Single-Drug, Open-Label, Pilot Study. Circulation 2005; 111: 3274-3280. [CrossRef] [PubMed]
DOI: https://doi.org/10.7199/ped.oncall.2013.53
|
| Cite this article as: | | Ghai A, Agrawal N, Rawal S. HYPERCAPNEA AND NON INVASIVE VENTILATION IN PRADER-WILLI SYNDROME. Pediatr Oncall J. 2013;10: 119-120. doi: 10.7199/ped.oncall.2013.53 |
|