Keywords
Subtle seizure, phenobarbitone, Neonate, EEG, Phenytoin
Introduction
Seizures constitute the most common neurological emergency in neonates. They have a significant impact on neonatal mortality as well as morbidities with adverse neurological outcomes.
Definition:
Any alteration in behavior, motor or autonomic neurologic function is defined as a seizure. It is further described as1:
- Epileptic seizures: clinical seizures associated with EEG changes
- Non-epileptic seizures: clinical seizures but no EEG manifestations
- EEG seizures: Abnormal EEG activity, no clinical seizures
Incidence:
True incidence is unknown. In terms of neonates, the estimated incidence is 1-5/1000 newborns whereas, in preterm neonates, the incidence is estimated at as high as 22%.2,3,4
Classification
All neonatal seizures are usually classified into one of the four categories as enumerated in Table 1 below.
Table 1: Clinical classification of seizures
| Seizure Type |
Incidence |
Clinical signs |
| Subtle |
Commonest (50%) |
Lip smacking
Sucking or swallowing movements
Pedaling, swimming
Horizontal or persistent deviation of eyes
Sometimes, apnea associated with eye or oral signs
|
| Tonic |
10-20% |
Sustained increase in muscle tone
Extension or flexion of limbs for few seconds to minutes
|
| Clonic |
10-20% |
Rhythmic muscle jerking in one or more body parts |
| Myoclonic |
Least common (1-2%) |
Lightning-like jerks of extremities
Non-rhythmic repetitive jerking in one or more body parts
|
Etiology
After a clinical diagnosis of seizure has been made, a detailed workup should be undertaken for underlying etiology, in particular the treatable causes. The antenatal, perinatal history and family history constitute the most important aspects of the initial evaluation. Common etiologies for neonatal seizures are Hypoxic ischemic encephalopathy (HIE), intracranial bleeds, metabolic disturbances (e.g. hypoglycemia, hypocalcemia, hyponatremia, etc) and intracranial infections.
Investigations
Next proceed with investigations to confirm the diagnosis, identify the etiology, and plan the management with anti-seizure drugs.
First line:
Blood glucose, calcium (ionic & total), serum sodium and an arterial blood gas
Second line:
Sick neonates with seizures should additionally undergo workup for sepsis (Sepsis screen & blood culture), intracranial infection (CSF studies to rule out meningitis), intracranial bleeding [cranial ultrasonography (CUS) & CT scan brain] and work up for inborn errors of metabolism wherever indicated.
Neuroimaging:
Neuroimaging helps to identify the etiology and the extent of severity of the insult.
- A bedside CUS should be done in all neonates with seizures to rule out intracranial bleeds, major malformations, and abscesses.
- Non-contrast CT can be performed to rule out subarachnoid/epidural hemorrhage.
- MRI is the preferred imaging modality to evaluate for the presence of ischemic stroke, brain malformations.
Role of EEG in Neonatal Seizures
Conventional video-EEG is the gold standard for neonatal seizure detection.5 It should be considered in all neonates to confirm the diagnosis, to identify the etiology and plan the management with anti-seizure drugs, to prognosticate the outcome, and to decide the course of antiepileptic medications. Whenever possible, it should be recorded close to the seizure episode. EEG should be recorded for at least a 1-hour duration.6
Treatment
No evidence-based guidelines exist currently for the management of neonatal seizures.7 Management of seizures includes stabilization, identification of the underlying cause, and specific treatment.
- Neonates with brief seizures due to transient, reversible electrolyte or glucose abnormalities do not require immediate treatment with anti-seizure drugs.
- All clinical seizures with EEG correlates and all EEG seizures should be aggressively treated with AED
- Clinical seizures that are prolonged (greater than 2 minutes) or that are frequent (greater than 3 episodes in 2 minutes) warrant treatment.
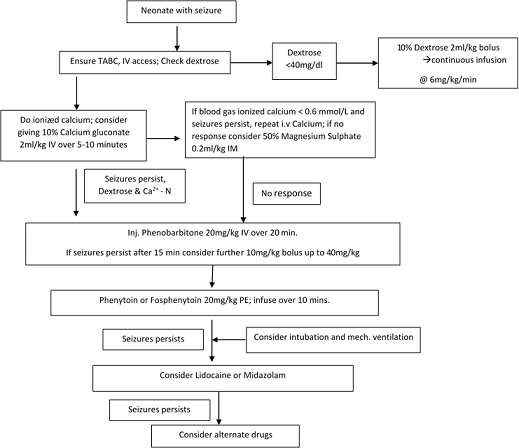
In practice, phenobarbital remains the drug of the first choice for confirmed or suspected seizures.8 The dose is 20 mg/kg/IV slowly over 20 minutes, with a maximum cumulative dose of 40 mg/kg (see Figure 1). If seizure persists despite a maximal dose of phenobarbitone, fosphenytoin (preferably) or phenytoin is indicated. The dose is 20 mg/kg IV under cardiac monitoring. Either midazolam or lidocaine may be used as third-line agents for seizures refractory to phenobarbital and/or phenytoin.
Figure 1: Immediate management of seizures including use if anti-seizure medications
Prognosis
Neonatal seizures are associated with high mortality and morbidity rates, with preterm babies even at higher risk of poor outcomes. Neonates with seizures have a risk for epilepsy (20-25%) during childhood.9
Indicators of poor outcomes in neonatal seizures:
- Refractory seizures
- Subtle or myoclonic form of seizures
- Abnormal neurological status before onset of seizures and after the seizures are controlled
- Cerebral dysgenesis, HIE III, meningitis, hypoglycemia
- EEG: low background activity or a burst suppression pattern
- Neuroimaging: deep grey matter/multifocal or diffuse cortical involvement
Long Term Management
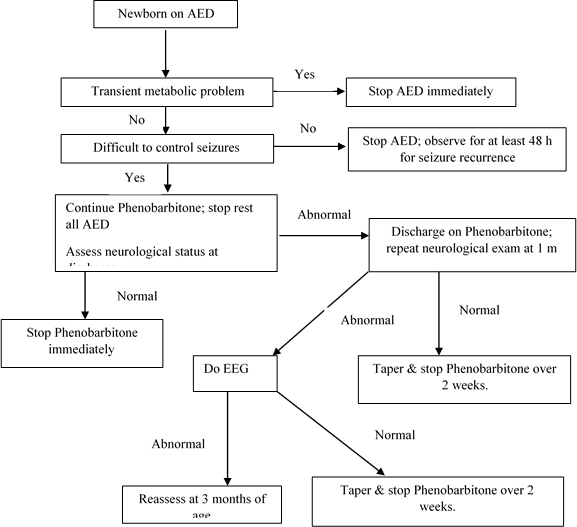
Neonatal seizures rarely reoccur during the first 2 years of life, and prophylactic antiepileptic drug administration need not be maintained past 3 months of age, even in the child at risk.10 Definite guidelines do not exist regarding the duration of anticonvulsant treatment for neonatal seizures. The protocol recommended by Volpe11 is usually followed at most places (See Figure 2).
Figure 2: Strategy to wean off AED in neonates
1. Mizrahi EM, Kellaway P. Characterization and classification. In Diagnosis and management of neonatal seizures. Lippincott-Raven, 1998; pp 15-35.
2. Ellenburg JH, Hirtz DG, Nelson KB. Age at onset of seizures in young children. Ann Neurol. 1984;15:127-34.
3. National Neonatal Perinatal Database. Report for year 2002-03. National Neonatology Forum, India.
4. Ronen GM, et al. The epidemiology of clinical neonatal seizures in Newfoundland: a population-based study. J Pediatr. 1999;134: 71-75.
5. Shellhaas RA, Chang T, Tsuchida T, Scher MS, Riviello JJ, Abend NS, et al. The American Clinical Neurophysiology Society's Guideline on Continuous Elec- troencephalography Monitoring in Neonates. J Clin Neurophysiol 2011;28: 611e7.
6. Wical BS. Neonatal seizures and electrographic analysis: evaluation and outcomes. Pediatr Neurol 1994;10:271-5.
7. Booth D, Evans DJ. Anticonvulsants for neonates with seizures. Cochrane Data- base Syst Rev 2004;(4):CD004218.
8. Clancy RR. Summary proceedings from the neurology group on neonatal seizures. Pediatrics 2006;117(3 Pt 2):S23e7.
9. Watanabe K, et al. Neonatal seizures and subsequent epilepsy. Brain Dev. 1982;4:341-346.
10. Hellstrom-Westas L, et al. Low risk of seizure recurrence after early withdrawal of antiepileptic treatment in the neonatal period. Arch Dis Child Fetal Neonatal Ed. 1995;72:F97-F101.
11. Volpe JJ. Neonatal Seizures. In Neurology of the newborn. Philadelphia: WB Saunders, 1999; 172-225.2. Ellenburg JH, Hirtz DG, Nelson KB. Age at onset of seizures in young children. Ann Neurol. 1984;15:127-34.
3. National Neonatal Perinatal Database. Report for year 2002-03. National Neonatology Forum, India.
4. Ronen GM, et al. The epidemiology of clinical neonatal seizures in Newfoundland: a population-based study. J Pediatr. 1999;134: 71-75.
5. Shellhaas RA, Chang T, Tsuchida T, Scher MS, Riviello JJ, Abend NS, et al. The American Clinical Neurophysiology Society's Guideline on Continuous Elec- troencephalography Monitoring in Neonates. J Clin Neurophysiol 2011;28: 611e7.
6. Wical BS. Neonatal seizures and electrographic analysis: evaluation and outcomes. Pediatr Neurol 1994;10:271-5.
7. Booth D, Evans DJ. Anticonvulsants for neonates with seizures. Cochrane Data- base Syst Rev 2004;(4):CD004218.
8. Clancy RR. Summary proceedings from the neurology group on neonatal seizures. Pediatrics 2006;117(3 Pt 2):S23e7.
9. Watanabe K, et al. Neonatal seizures and subsequent epilepsy. Brain Dev. 1982;4:341-346.
10. Hellstrom-Westas L, et al. Low risk of seizure recurrence after early withdrawal of antiepileptic treatment in the neonatal period. Arch Dis Child Fetal Neonatal Ed. 1995;72:F97-F101.
11. Volpe JJ. Neonatal Seizures. In Neurology of the newborn. Philadelphia: WB Saunders, 1999; 172-225.