|
Sacral Lesions
Sofia Reis1, Paulo Morais2.
1Department of Pediatrics, Tondela-Viseu Hospital Center, Viseu, Portugal,
2Department of Dermatology, Tondela-Viseu Hospital Center, Viseu, Portugal.
ADDRESS FOR CORRESPONDENCE
Sofia Reis, Department of Pediatrics, Av. Rei D. Duarte, 3504-509 Viseu, Portugal.
Email: reis.carlasofia@gmail.com
|
|
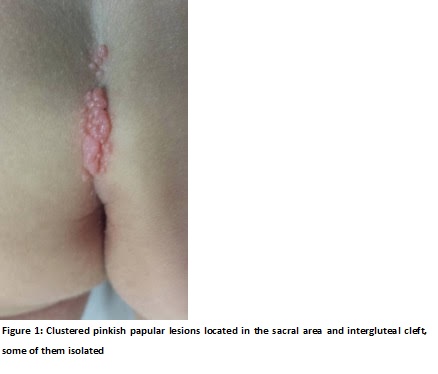
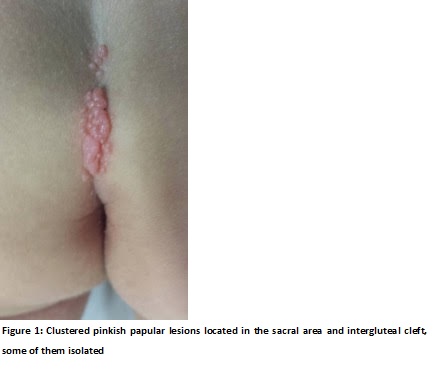
Is it molluscum contagiosum infection or condyloma acuminata?
The lesions were treated by curettage and application of trichloroacetic acid with complete resolution. The histological examination of the lesions obtained by curettage revealed lobulated, endophytic epidermal hyperplasia with intracytoplasmic molluscum bodies confirming the diagnosis of MC. Thus, the diagnosis of agminated MC with condyloma-like appearance was established.
Molluscum contagiosum results from keratinocytes infection by a poxvirus, the MC virus. It is usually a benign disease, common in childhood, with outbreaks often associated with attendance at swimming pools. The diagnosis of MC is clinical and epidemiological. (1-3) Characteristically, the lesions are isolated, umbilicated papules filled with a gelatinous and sticky mass, more commonly located in the areas of friction from clothing, rubbing the skin such as the neck, armpit and upper body. (1) MC lesions are usually asymptomatic` however, itching or tenderness may be present. (2) Sometimes, the lesions may form clusters or present in atypical location, size, number and configuration, making the diagnosis not so clear, like this case. Plaques composed of many small confluent, or agminated, lesions were described by Bunch, in 1918. (4) The ‘agminate’ variety and other atypical forms (e.g, giant and verrucous forms) of MC occur rarely. (5) On the other hand, anogenital MC is rare in children. (6) In a child who has only anogenital involvement, one would have increased suspicion of sexual abuse. (7) In our patient, detailed inquiry revealed no evidence of child abuse, and transmission was assumed to be from his older brother.
Treatment of MC infection is not mandatory considering its possible spontaneous remission in a healthy child. (3) However, treatment prevents seed by autoinoculation, perpetuation of the disease and potential complications, including irritation, inflammation or secondary infection. (2) The choice of treatment will depend on the patient’s age, and the number and location of the lesions. Treatment options include: a) caustic destruction with cantharidin, trichloroacetic acid or diluted liquefied phenol; b) irritant agents, such as potassium hydroxide, salicylic acid, retinoids, and others; c) surgical irritation (squeezing, insertion of pointed stick); d) surgical treatments, including curettage, cryotherapy and lasers; e) immune response enhancers, such as imiquimod cream, topical diphencyprone or systemic cimetidine; f) intravenous or topical cidofovir. (5) |
| |
| Compliance with ethical standards |
|
Funding: None
|
|
|
Conflict of Interest: None
|
|
- Leung AKC. The natural history of molluscum contagiosum in children. Lancet Infect Dis. 2015;15:136-7. [CrossRef]
- Olsen JR, Gallacher J, Finlay AY, Piguet V, Francis NA. Time to resolution and effect on quality of life of molluscum contagiosum in children in the UK: a prospective community cohort study. Lancet Infect Dis. 2015;15:190-5. [CrossRef]
- Chen X, Anstey AV, Bugert JJ. Molluscum contagiosum virus infection. Lancet Infect Dis. 2013;13:877-88. [CrossRef]
- Bunch JL. Agminated Molluscum Contagiosum. Proc R Soc Med. 1918;11(Sect Study Dis Child):44.
- Sterling JC. Viral infections. In: Burns DA, Breathnach SM, Cox N, Grifiths C.(eds). Rook Textbook of Dermatology. 7th Edition. Oxford: Blackwell Scientiic Publications Ltd. 2004;25.1-25.95. [CrossRef]
- Zhuang K, Ran Y, Xu F, Lama J. Atypical infantile genital Molluscum contagiosum. An Bras Dermatol. 2015;90: 403–5. [CrossRef] [PubMed] [PMC free article]
- Bargman H. Is genital molluscum contagiosum a cutaneous manifestation of sexual abuse in children? J Am Acad Dermatol. 1986;14(5 Pt 1):847–9. [CrossRef]
|
|
DOI: https://doi.org/10.7199/ped.oncall.2017.44 |
| |
Cite this article as:
Reis S, Morais P. Sacral Lesions (Agminated Molluscum Contagiosum with Condyloma-Like Appearance). Pediatr Oncall J. 2017;14: 98. doi: 10.7199/ped.oncall.2017.44
|