Sara Oliveira, Sara Isabel de Almeida, Sílvia Batalha, Joana Rios, Paulo Oom.
Pediatric Department, Hospital Beatriz Ângelo, Loures, Portugal.
ADDRESS FOR CORRESPONDENCE
Sara Isabel Alves Baptista de Oliveira, Pediatric Department of Hospital Beatriz Ângelo; Hospital Beatriz Ângelo, Avenida Carlos Teixeira, 3 - 2674-514 Loures, Portugal.
Email: sara.oliveira@hbeatrizangelo.pt | | Abstract | The new onset of abdominal pain in a constipated patient is usually related to this problem but we should keep in mind differential diagnosis.
A 9-year-old girl with history of alopecia, iron deficiency anemia and constipation, presented to the emergency department with colic epigastric pain, anorexia, vomiting, no emission of stools and no fever. She appeared pale and malnourished. The evaluation revealed a painless, hard, palpable mass in the epigastric region.
Abdominal ultrasound evaluation was limited by gas trapping. The abdominal CT scan revealed an ileoileal intussusception and a gastric heterogeneous endoluminal mass, identified in the upper gastrointestinal endoscopy as a large trichobezoar, only possible to remove with gastrotomy. Another small bezoar at the jejunal level conditioned intussusception, treated with resection and anastomosis.
Trichobezoars are rare in childhood. In most cases, as in this one, it reveals a psychiatric disorder that must be treated to prevent recurrence. | | | | Keywords | | Constipation, intussusception, bezoar | | | | Case Report | A 9 years old female presented to the pediatric emergency department (PED) with a two day history of colic epigastric pain, anorexia and no stool emission. She was prescribed a laxative and discharged home after symptom relief. Three days later she returned to PED with worsening symptoms and also reporting vomiting after every meal. She denied fever or other symptoms.
Her previous medical history revealed a dermatologic evaluation at 3 years old due to alopecia without further follow-up. A previous history of constipation and an iron deficiency anemia diagnosed at 6 years old and supplemented with oral iron was also referred, but with irregular follow-up by her family physician.
Familial and social history revealed five older brothers and sisters, two of them living in a foster home. She was currently the only one living with her mother and she had no contact with her father. She was attending the second grade of primary school with good grades, even though there was a history of problems with her peers.
On physical examination she adopted an antalgic positioning during walk and on standing position, with a pale and malnourished appearance. She weighed 26 kilograms and her body mass index was 19.3 kg/m2. Abdominal evaluation revealed a painless and hard palpable mass in the right epigastric and hypochondriac regions; the remainder of the examination was normal.
Initial blood assessment revealed iron deficiency anemia (hemoglobin 11.7 g/dL, ferritin 12.1 μg/dL) and an elevated lactate dehydrogenase (411 UI/L) and C-reactive protein (3.32 mg/dL). Abdominal ultrasound showed perihepatic ascites and gas trapping.
Considering her past history and initial work-up, the diagnosis of serious constipation was assumed and medical disimpaction treatment was optimized.
After medical disimpaction she maintained abdominal complaints and there was no stool emission. For that reason, she was admitted to further investigation and treatment.
An abdominal CT scan was performed revealing an ileoileal intussusception and a bulky heterogeneous endoluminal mass in the stomach of undetermined nature (Figure 1). The upper gastrointestinal (UGI) endoscopy identified a large trichobezoar whose removal could only be possible with gastrostomy due to its width (Figures 2 and 3).
Figure 1. CT images demonstrating an endoluminal mass in the stomach (asterisk in the left image) and an ileoileal intussusception (arrow in the right image).
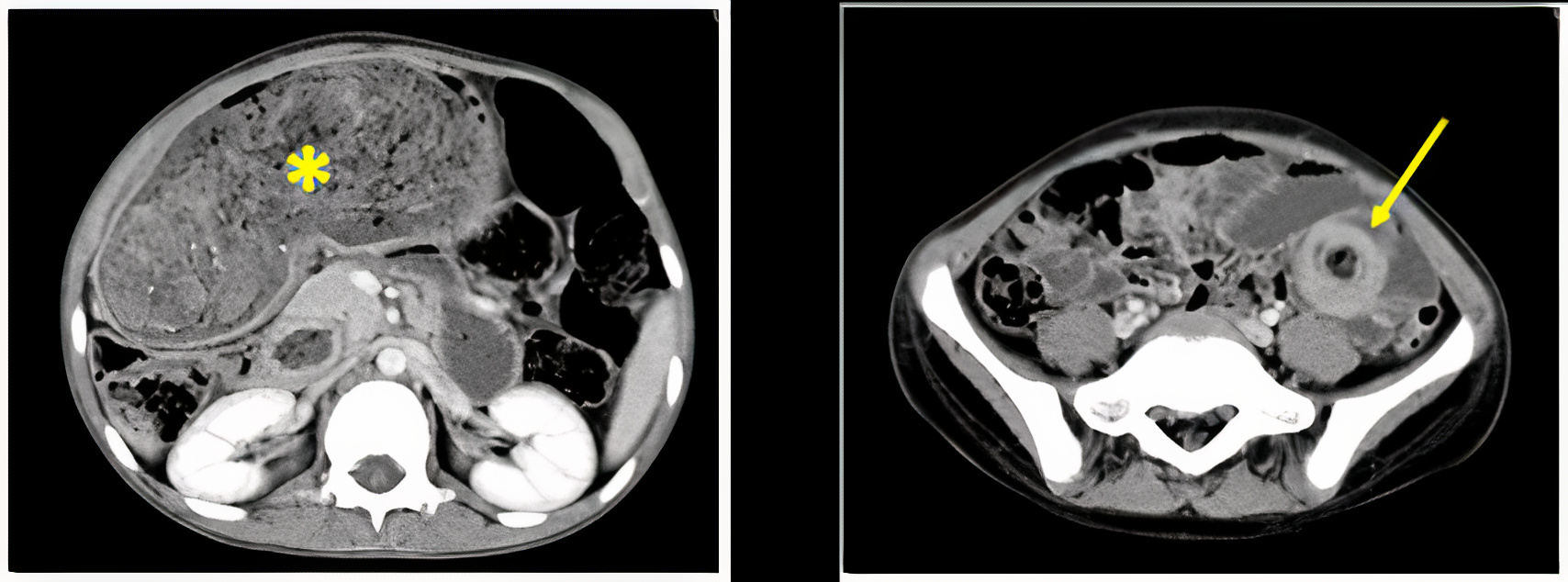
Figure 2. UGI endoscopy showing a large mass of hair.
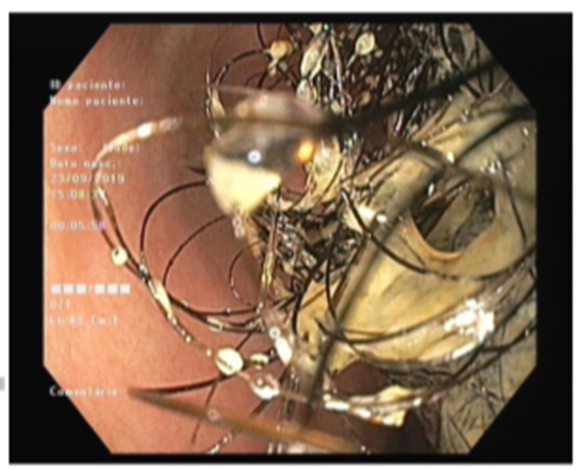
Figure3. Large trichobezoar removed with a gastrotomy.

On day 3 of admission, she was submitted to surgery for removal and the intussusception was found due to presence of a small bezoar. Consequently, a resection and top-to-top anastomosis was performed. Six days after surgery, she started with fever, prostration and pain in the hypogastric region. No urinary or gastrointestinal symptoms were noticed. An abdominal ultrasound revealed intra-abdominal fluid collection in the Douglas sac, compatible with an abscess. She underwent a laparotomy to drain the abscess and was started on broad spectrum antibiotic therapy with piperacillin-tazobactam and amikacin during 14 days.
Clinical and nutritional improvement were noticed in the following days.
During the hospital stay, a past history of trichotillomania and trichophagia, as well as ingestion of objects such as wood pencils, was revealed by her mother. The investigation of the context revealed a history of bullying at school in the past two years.
Additionally, there was a notorious absence of her mother during the hospital stay, which exacerbated her depressive and anxious mood with periods of crying and emotional distress every time her mother left. She also started to have nocturnal enuresis during admission. The social service reported an absent mother and an unstructured family and the psychiatry confirmed the diagnosis of depressive humor and anxiety related to her family situation.
She started psychotherapy along with treatment with daily risperidone and diazepam as needed, with obvious clinical improvement.
She also had diet enrichment and started polymeric supplements to help the recovery of her nutritional status, with successful weight gain.
Two months after admission she was discharged to a foster home. She keeps having regular psychological as well as pediatric, nutritional and psychotherapy appointments. The clinical improvement is evident, including behavior and anxiety control, which continues to be worked out.
| | | | Discussion | Gastrointestinal bezoars are poorly or non-digested congregations or compact masses. They can be formed by a variety of materials, including ingested hair – trichobezoars.1,2
The mucosal folds of the stomach are the most common place of formation because of the natural blockage to further passage in the pylorus. In some cases there can be an extension of the hair into other parts of the intestine, the well described Rapunzel Syndrome. If some part breaks and migrate into the small intestine, it can cause intestinal obstruction.3,4
They are quite uncommon in the pediatric age group and usually found in females in the second and third decades of life but can also present in children, especially in adolescents. Psychiatric disorders, a history of developmental delay and a disrupted familiar environment are strongly associated. Most patients have a history of trichotillomania, 30% of those will also have trichophagia and only 1% of these last patients develop a trichobezoar that requires surgical extraction.5
Depending on the size, location and the chronicity of the bezoar, it can originate numerous complications like small bowel intussusception, peritonitis, ulceration, anemia, severe malnutrition and others.
A palpable abdominal mass, typically in the epigastric region, stands out in 80% of the patients with a bezoar. However, without distinctive characteristics on palpation, it is difficult to differentiate between a possible hepatomegaly or colic cord, as was initially seen in our patient who had a previous history of constipation.6 In this scenario, such a common complaint like constipation, when associated with other non-completely understood symptoms like iron deficiency anemia, severe abdominal pain, abdominal mass and a compromise in child's development and nutritional status, should urge the pediatrician to think “outside the box” and consider less common diagnosis.
The gold standard for both diagnostic and therapeutic purposes is UGI endoscopy.1,7 When the endoscopic fragmentation/removal or the enzymatic dissolution are not possible, laparotomy is the most commonly performed procedure.
The CT scanning is useful to detect both gastric and small intestinal bezoars. It also allows the assessment of adjacent structures, the evaluation of the location and extent of the bezoar and the existence of complications, permitting accurate preoperative planning.8
A very similar case of a 7-year-old girl is documented, also with a history of trichotillomania and trichophagia that seemed to occur in response to physical fatigue.3
Another case of Rapunzel syndrome is described in the literature, in a 5-year-old girl with pica, also with a large trichobezoar found in the UGI endoscopy.7
Our case also highlights the importance of considering psychosocial history in cases with unusual findings.
All three cases demonstrate the importance of a multidisciplinary approach when treating this pathology to resolve the organic problem and also to promote nutritional recovery and psychological follow-up.
Our patient imposed a multidisciplinary approach of pediatricians, gastroenterologists, pediatric surgeons, nutritionists and psychology.
This patient is one of the few documented cases of children younger than 10 years old having a trichobezoar and is even more unique if we consider the passage of the bezoar into the small bowel causing an acute small bowel obstruction.
She also accounts for the about five documented cases of children diagnosed with a trichobezoar in Portugal, to our knowledge.
Learning points:
· Although most cases of abdominal pain in a patient with a previous history of constipation are due to an exacerbation of their pathology, other diagnosis should be considered, especially if there is a compromise of the child´s development and nutritional status.
· Trichobezoars are rare in children, particularly under 10 years old, but this diagnosis should be investigated if there is a history of alopecia, constipation and in a context of a dysfunctional family and psychiatric disorders.
· The treatment should include, not only trichobezoar removal, but also social evaluation and intervention, psychotherapy and nutritional rehabilitation.
· Multidisciplinary approach and familiar stability are crucial for clinical recovery. | | | | Compliance with Ethical Standards | | Funding None | | | | Conflict of Interest None | | |
| Cite this article as: | | Oliveira S, Almeida S I d, Batalha S, Rios J, Oom P. Abdominal pain: beyond the obvious. Pediatr Oncall J. 2024;21: 115-117. doi: 10.7199/ped.oncall.2024.24 |
|