Cheek cysticercosis - To Treat or Not to Treat
|
|
Cheek cysticercosis - To Treat or Not to Treat
31/08/2024
31/08/2024
https://www.pediatriconcall.com/Journal/images/journal_cover.jpg
Dhruv Gandhi1, Shatakshi Garg1, Zahabiya Nalwalla1, Balagopal Kurup2, Tejas Athalye2, Sunita Sharma3, Ira Shah1.
1Department of Pediatric Infectious Diseases, B J Wadia Hospital for Children, Mumbai, India,
2Department of ENT, B J Wadia Hospital for Children, Mumbai, India,
3Department of Pathology, B J Wadia Hospital for Children, Mumbai, India.
ADDRESS FOR CORRESPONDENCE
Dhruv Gandhi, 5B/13 Shyam Niwas, Breach Candy, Mumbai-400026, India.
Email: dhruvgandhi2610@gmail.com
Cheek cysticercosis, oral cysticercosis, cysticercosis cellulosae, Taenia solium, pig tapeworm, cheek swelling
|
Clinical Problem
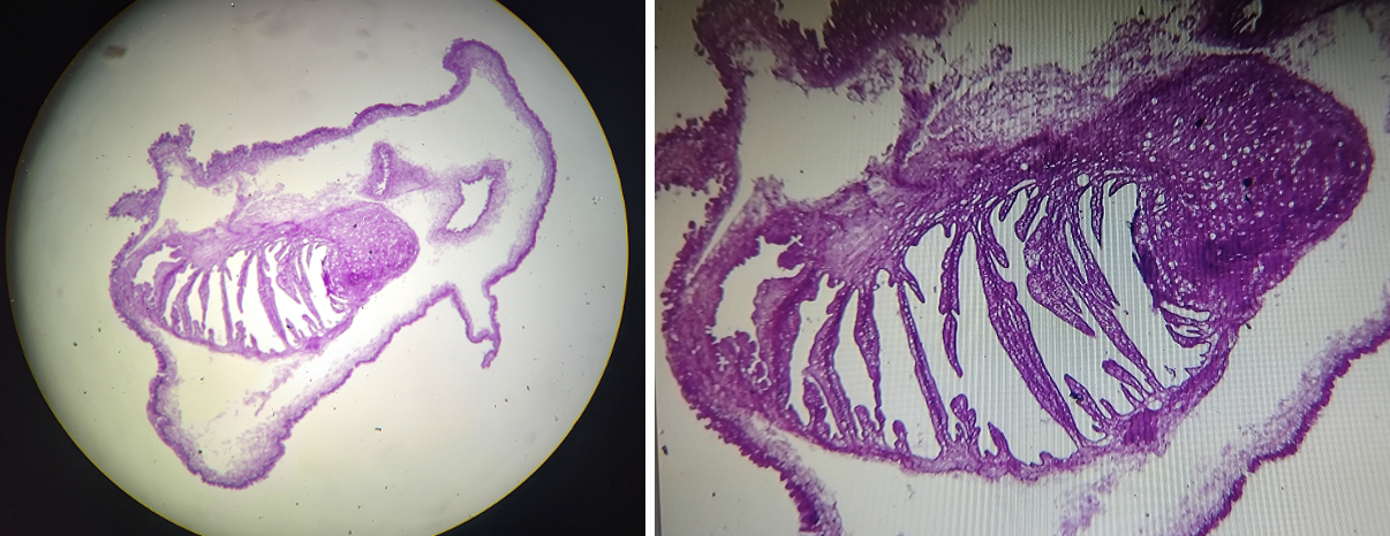
A 14-year-old boy presented with a painless, progressively enlarging right cheek swelling for six months. There was no fever or trauma. He had a mixed dietary pattern. On examination, there was a solitary, non-tender, freely mobile, well-defined, smooth, firm swelling in the right cheek measuring approximately 1.5 X 1.0 cm. Oral cavity examination was normal. Other systemic and general examination were normal. Ultrasonography (USG) of the cheek showed an intramuscular well defined cystic lesion measuring 1.4 X 1.2 mm with a central echogenic focus measuring 0.3 X 0.2 mm and thin septae suspicious of a dermoid cyst or epidermal inclusion cyst. Surgical excision of the cyst was performed. On microscopic examination, an undulating cyst wall resting on skeletal muscle and adipose tissue and lined by foamy histiocytes was seen. The separate soft tissue mass on sectioning revealed irregularly shaped membranous infoldings representing cysticercus larvae. Histopathology was suggestive of cysticercus cellulosae of the cheek (Figure 1). Subsequently, a magnetic resonance imaging (MRI) brain was done to rule out neurocysticercosis which was normal and ophthalmology examination was also normal.
Figure 1. Histopathology showing an ulcerated cyst wall suggestive of cysticercus cellulose.
|
| |
Should the child be treated with antihelminthics?
|
|
|
Discussion
Pediatric cheek swellings can be attributed to various causes including lymphadenopathy, abscesses, odontogenic infections, neurofibromas, lymphangiomas and tumors.1 Of these, a rare cause of a slowly progressive cheek swelling is cysticercosis cellulosae caused by the larval stage of the pig tapeworm, Taenia solium. Cysticercosis is caused by a parasitic cestode belonging to Phylum Platyhelminthes. This tapeworm has a two host life cycle with the definitive host being humans who harbor the worms and the intermediate host being pigs who harbor the larvae. On consumption of improperly cooked or raw pork, the larvae present in the meat hatch to form the adult worms in the small intestine. This infestation is known as taeniasis.2,3,4 Human cysticercosis, on the other hand, is a larval infestation in which humans are the intermediate hosts. Eggs passed out in feces may contaminate food, water or hands and thus may be ingested by humans.2,3,4, These eggs form larvae in the intestine following which they penetrate the mucosa to reach the blood vessels and lymphatics. They are then transported to various organs particularly the brain, lungs, heart, skeletal muscles and skin. These larvae eventually die triggering a foreign body reaction with granuloma formation, fibrosis and calcification about 3 months later. These lesions are known as cysticerci.4
Oral cysticercosis is a rare presentation with less than a hundred cases reported in literature at present.2,5 A case-based review has found that the tongue is the most common site of predilection, accounting for about 50% of the cases followed by the labial and buccal mucosa.2 Cheek cysticercosis with the involvement of masseter or buccinator muscles has been reported in a small minority of cases.3,5,6,7,8,9
Intramuscular cysticercosis may be classified into three types based on their clinical presentations. Firstly, the myalgic type, in which the death of the larva and subsequent cyst fluid leakage triggers acute inflammation presenting as severe localised pain. The mass-like, pseudotumor-like or abscess-like type, in which intermittent cyst fluid leakage and collection around the cyst leads to chronic inflammation and presents with a mass lesion. Lastly, the pseudohypertrophic type, in which the scolex calcifies and the capsule retracts and thickens.2 Differential diagnoses include mucocoele, lipoma, fibroma, hemangioma, neurofibroma, dermoid cyst, epidermoid cyst and salivary gland tumors.1,2 Our patient had a mass-like cheek cysticercosis.
Diagnosis can be made on imaging in most cases with confirmation by histopathological examination.2,6,7 USG has four distinct pathognomonic appearances of intramuscular cysticerci: cyst surrounded by an inflammatory mass; irregular cyst surrounded by minimal fluid at one end; large irregular exudative fluid collection with an eccentrically located cyst within this collection; and elliptical calcified cysts resembling millet seeds.2,6,7 Magnetic resonance imaging (MRI) can visualise active and degenerating cysticerci well whereas computerised tomography (CT) can visualise calcified cysticerci well.2
Fine-needle aspiration cytology (FNAC) can be used to detect the larval fragments which contain multiple ovoid nuclei in a fibrillary stroma surrounded by a light-stained undulating membrane. Typically, the aspirate contains pearly white lesions which represent the larvae. Histopathological examination shows larvae within the tissue or scolices within the cysts.2
Treatment of oral cysticercosis depends upon the disease activity and the location of the cysts.2,3 Inactive cysts do not require treatment. Medical management with antihelminthics such as albendazole at a dose of 15 mg/kg/day for 8 days or praziquantel at 50 mg/kg/day in three divided doses for 15 days is effective in the treatment of cysticercosis.3 Surgical excision is also a favourable treatment modality for oral cysticercosis due to their superficial location and well-localised lesions. Surgical excision may be done for tissue diagnosis, cosmetic reasons or for lesions causing discomfort.2,8,9
The dilemma of choosing to treat with antihelminthics in such cases is a unique one. Chand et al.5 and Mittal et al.6, chose sole conservative management in their respective cases as USG findings were highly suggestive of cysticercosis in both, hence surgical excision for tissue diagnosis was not needed. Similarly, Dysanoor et al.9, initially managed their case medically as USG findings were highly suggestive of cysticercosis. Ramakrishnan et al.7 chose sole conservative management as FNAC confirmed the diagnosis of cysticercosis. Krishnamoorthy et al.2, did administer antihelminthics post-excision as they were not able to rule out the presence of neurocysticercosis due to patient unaffordability for neuroimaging.
In our case, since the diagnosis was not confirmed on USG, we went for surgical excision to obtain a tissue diagnosis. Other factors favouring surgical management in this patient include the solitary nature of the lesion and the possibility of complete excision. Following excision, we chose not to treat our patient with antihelminthics as there was no presence of cysticercosis in the eye or the brain.
|
| |
| Compliance with ethical standards |
|
Funding: None
|
|
|
Conflict of Interest: None
|
- Khanna G, Sato Y, Smith RJ, et al. Causes of facial swelling in pediatric patients: correlation of clinical and radiologic findings. Radiographics. 2006 Jan-Feb;26(1):157-71. doi: 10.1148/rg.261055050. PMID: 16418250. [CrossRef] [PubMed]
- Krishnamoorthy B, Suma GN, Dhillon M, et al. Encysted Tenia solium larva of oral cavity: Case report with review of literature. Contemp Clin Dent. 2012 Sep;3(Suppl 2):S228-32. doi: 10.4103/0976-237X.101103. PMID: 23230370; PMCID: PMC3514943. [CrossRef] [PubMed] [PMC free article]
- Gautam S, Patnaik M, Singh HP, et al. Cysticercosis of cheek as a rare presentation: Case report and review of literature. The Egyptian Journal of Otolaryngology. 2022 Jul 29;38(1). doi:10.1186/s43163-022-00286-y [CrossRef]
- Hosur MB, Byakodi S, Puranik RS, et al. Oral Cysticercosis: A Case Report and Review of Literature. J Maxillofac Oral Surg. 2015 Sep;14(3):853-7. doi: 10.1007/s12663-015-0745-x. Epub 2015 Jan 30. PMID: 26225089; PMCID: PMC4511908. [CrossRef] [PubMed] [PMC free article]
- Chand S, Mishra M, Singh G, et al. Orofacial cysticercosis: Report of a rare case with review of literature. Natl J Maxillofac Surg. 2016 Jul-Dec;7(2):209-212. doi: 10.4103/0975-5950.201353. PMID: 28356697; PMCID: PMC5357924. [CrossRef] [PubMed] [PMC free article]
- Mittal A, Das D, Iyer N, et al. Masseter cysticercosis - a rare case diagnosed on ultrasound. Dentomaxillofac Radiol. 2008 Feb;37(2):113-6. doi: 10.1259/dmfr/31885135. PMID: 18239039. [CrossRef] [PubMed]
- Ramakrishnan P, Bahirwani S, Balaji P. Cysticercosis of the masseter. Indian J Dent Res. 2012 May-Jun;23(3):436. doi: 10.4103/0970-9290.102258. PMID: 23059599. [CrossRef] [PubMed]
- Riju JJ, Shiva Kumar AM, Sashikala P. Cysticercosis of Cheek: A CaseReport. J Microbiol Pathol. 2018;2:109.
- Dysanoor S, Pol J. A solitary facial nodular swelling - A case report of intramuscular cysticercosis in buccinator muscle. Asian Pac J Trop Dis. 2013 Jun;3(3):235-9. doi: 10.1016/S2222-1808(13)60047-X. PMCID: PMC4027287. [CrossRef]
|
|
| |
Cite this article as:
Gandhi D, Garg S, Nalwalla Z, Kurup B, Athalye T, Sharma S, Shah I. Cheek cysticercosis - To Treat or Not to Treat. Pediatr Oncall J. 2024;21: 193-194. doi: 10.7199/ped.oncall.2024.51
|