Jeslyn Tengkawan1, Titi Pambudi Karuniawaty2, Zulfikar Ihyauddin1, Ayu Anandhika Septisari1.
1Yayasan Capella Project Indonesia, Indonesia,
2Department of Child Health, Faculty of Medicine, Mataram University, West Nusa Tenggara, Indonesia.
ADDRESS FOR CORRESPONDENCE
Jeslyn Tengkawan, Yayasan Capella Project Indonesia, Taman Surya 5 Ruko Avenue Blok KK1 No. 57, Cengkareng, Jakarta Barat, Indonesia 11730.
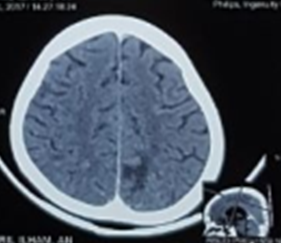
Email: jeslynteng@yahoo.com | | Abstract | | Hemorrhagic transformation in embolic stroke is a rare complication of rheumatic heart disease (RHD) that usually happens in old age. A 10-year-old boy suffering from RHD since 2016 was hospitalized with an exacerbation of rheumatic fever (RF) and poor medication compliance. On his seventh day of hospitalization, he had tension headache followed by a tonic-clonic seizure and sudden bilateral vision loss. The brain CT-scan brain showed intracranial hemorrhage with perifocal edema, ischemic process, and ventriculomegaly on the lateral ventricle. Symptoms completely resolved after the 16th day of hospitalization. | | | | Keywords | | hemorrhagic transformation, embolic stroke, rheumatic heart disease, pediatrics | | | | Introduction | | Rheumatic heart disease (RHD) is a common consequence of acute rheumatic fever (ARF) in developing countries.1 The incidence of stroke in RHD patient is 43 per 100,000 according to Iran stroke registry.2 Meanwhile, the incidence of hemorrhagic stroke in RHD patients is still not clearly determined. In this case report, we present a ten years old boy with RHD who presented with acute rheumatic fever (ARF) and hemorrhagic transformation of embolic stroke. | | | | Case Report | A 10-years-old boy suffering from RHD since June 2016 was hospitalized in December 2017 with exacerbation of ARF. He presented with fever for four weeks, pain, redness, swelling, and stiffness of large joints especially in the left knee, fatigue, and dyspnea. He had not been taking his medications after the diagnosis in June 2016. On presentation, the boy’s body weight was 26 kg with blood pressure 110/75 mmHg, heart rate 120/min, and temperature 39.8oC. There was a systolic murmur on the left parasternal fourth intercostal space. Laboratory studies showed hemoglobin 4.5 g/dL, white cell count (WBC) 33,940 cells/cumm, platelets of 890,000 cells/cumm, C-reactive protein (CRP) 239.7 mg/dl, Anti-Streptolysin O (ASLO) 200 IU/mL, negative antinuclear antibodies test (ANA), SGOT 31 mg/dL, SGPT 29 mg/dL, urea 18 mg/dL, creatinine 0.27 mg/dL, sodium 131 mmol/L, potassium 3.6 mmol/L, and chloride 100 mmol/L. Electrocardiogram (ECG) showed sinus tachycardia and no prolonged PR interval. A chest X-ray showed cardiomegaly with CTR of 0.6 (Figure 1), while echocardiography showed trivial tricuspid regurgitation with an ejection fraction of 61.04%. He was diagnosed as ARF with RHD and heart failure with severe anemia. He was transfused with 750 mL of packed red blood cells (PRBC), and given intravenous (IV) ceftriaxone, oral erythromycin, oral prednisone, and oral aspirin for six days. On day seven of hospitalization, he complained of neck pain followed by a tonic-clonic seizure that lasted for 5 minutes which was aborted by IV diazepam. Blood pressure was 170/100 mmHg, heart rate was 152/min, oxygen saturation of 89%. After gaining full consciousness, the patient complained of sudden vision loss with a visual acuity of 1/300 in both eyes. A blood sample showed no electrolyte or blood glucose abnormalities. CT-Scan showed intracranial hemorrhage in the left parietal lobe with perifocal edema and ischemic process, and also ventriculomegaly on the lateral ventricle (Figure 2). Two-hours after administration of 20 mg of nifedipine via nasogastric tube, blood pressure decreased to 110/70 mmHg. The patient was given 75 mg of phenobarbital twice a day as prophylaxis for seizures. Four hours later, his blood pressure increased to 140/110 mmHg, he was given captopril 12.5 mg every 12 hours. There was no recurrence of seizure and his blood pressure was within normal limits. His vision got better in three days. The patient was discharged after sixteen days of hospitalization without any complaints.
Figure 1. Chest X-ray showing cardiomegaly
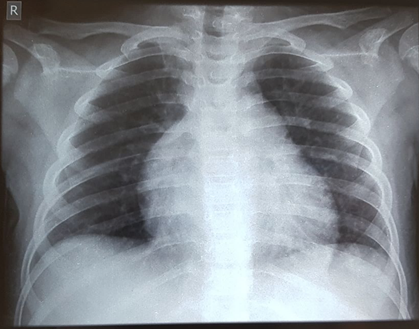
Figure 2. CT Scan brain shows hyper-density in left parietal lobe with hypodense lesion.
 | | | | Discussion | Infections by Group A streptococcus (GAS) causes an autoimmune reaction known as ARF which leads to a chronic cardiac condition well known as RHD.3 Common complications of RHD are congestive heart failure and stroke, affecting one-fifth of patients over two years.4 The association between stroke and RHD is higher for RHD patients who also have atrial fibrillations, increasing the risk of stroke until 18-times higher.5 In RHD, emboli formation could happen as a consequence of the calcification process that is undergone by the rheumatic valves.6 When released, it might flow to the brain resulting in a cardioembolic stroke, which is responsible for approximately 14-30% of all cerebral infarction cases.7 Although it is clear that RHD usually affects mitral and aortic valves,3 our case presented a rare manifestation in which the tricuspid valves were affected, resulting in a trivial tricuspid regurgitation showed by an echocardiography examination. A study by Sultan et al. reported that rheumatic tricuspid valve disease is often undetected and overlooked in RHD patients, in which in their study this case occurred in approximately 7.7% patients with RHD, detected using echocardiographic examination.8 Transient vision loss in children with ARF is relatively rare and has not been described well. In our patient, transient vision loss was suspected due to retrobulbar neuritis which could be caused by disturbance of retinal arterial flow or vasospasm due to micro-emboli in response to valve disturbance.9
Hemorrhagic transformation of stroke could occur as a complication in 10% of patients with ischemic stroke.10 Usually, the risks factors of hemorrhagic transformation are older age and large-sized infarct, but in our patient, it happened in the pediatric patient with small infarct but may be related to hypertension.11 Most of the hemorrhagic transformation with ischemic stroke occur within 30 days and are petechial and asymptomatic.12 According to the scientific statement from the American Heart Association/American Stroke Association (AHA/ASA), acute management of pediatric hemorrhagic stroke include patient stabilization, diagnosis establishment, and secondary neurological injury prevention. In cases where there is a significant increase of intracranial pressure, an external ventricular drain along with head elevation, hyperventilation, hyperosmolar therapy, and sedation should be carried out, while also considering surgical decompression as the ultimate option when it is necessary.13 In addition, standard therapy of RHD including antimicrobial therapy, suppression of the inflammatory process using an optimal dose of aspirin, and management of heart failure by using diuretics, angiotensin-converting enzyme inhibitors, or digoxin are recommended.14,15
The average mortality rate from hemorrhagic stroke in children is estimated to be 25% according to a pooled data from multiple heterogeneous studies, and ranging from 4% to 54% according to AHA/ASA.13,16 Developing epilepsy is one of the prominent sequels from pediatric hemorrhagic stroke, which could be observed in 4% of patients in their first year of follow up, and increased into 13% in the second year following the hemorrhagic stroke.17 | | | | Contributor Statement | | JT and TPK drafted the initial manuscript, reviewed and revised the manuscript. ZI and AAS reviewed and revised the manuscript. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work. | | | | Compliance with Ethical Standards | | Funding None | | | | Conflict of Interest None | | |
- Carapetis JR. Rheumatic Heart Disease in Developing Countries. N Engl J Med. 2007; 357:439-41. [CrossRef] [PubMed]
- Carapetis JR. Rheumatic Heart Disease in Asia. Circulation. 2008;118:2748-53. [CrossRef] [PubMed]
- Katzenellenbogen JM, Ralph AP, Wyber R, Carapetis JR. Rheumatic heart disease: infectious disease origin, chronic care approach. BMC Health Serv Res. 2017;17:793. [CrossRef] [PubMed] [PMC free article]
- Zühlke L, Karthikeyan G, Engel ME, Rangarajan S, Mackie P, Cupido-Katya Mauff B, et al. Clinical Outcomes in 3343 Children and Adults With Rheumatic Heart Disease From 14 Low- and Middle-Income Countries: Two-Year Follow-Up of the Global Rheumatic Heart Disease Registry (the REMEDY Study). Circulation. 2016;134:1456-66. [CrossRef] [PubMed]
- Wang D, Liu M, Lin S, Hao Z, Tao W, Chen X, et al. Stroke and rheumatic heart disease: A systematic review of observational studies. Clin Neurol Neurosurg. 2013;115:1575-82. [CrossRef] [PubMed]
- Rajamannan NM, Nealis TB, Subramaniam M, Pandya S, Stock SR, Ignatiev CI, et al. Calcified Rheumatic Valve Neoangiogenesis Is Associated With Vascular Endothelial Growth Factor Expression and Osteoblast-Like Bone Formation. Circulation. 2005;111:3296-301. [CrossRef] [PubMed] [PMC free article]
- Arboix A, Alioc J. Cardioembolic Stroke: Clinical Features, Specific Cardiac Disorders and Prognosis. Curr Cardiol Rev. 2010;6:150-61. [CrossRef] [PubMed] [PMC free article]
- Sultan FAT, Moustafa SE, Tajik J, Warsame T, Emani U, Alharthi M, et al. Rheumatic Tricuspid Valve Disease: An Evidence-Based Systematic Overview. J Heart Valve Dis. 2010;19:10.
- Mantagos IS, Rhodes J, Dagi LR. Transient Monocular Vision Loss from Acute Rheumatic Fever. Pediatr Cardiol. 2008;29:966-8. [CrossRef] [PubMed]
- Moncayo-Gaete J, Bogousslavsky J, Levine SR. Hemorrhagic transformation of ischemic stroke [Internet]. Neurology Medlink. 2019 [cited 2019 Aug 18]. Available from: https://www.medlink.com/index.php/article/hemorrhagic_transformation_of_ischemic_stroke
- Al-Farsi K, Siddiqui AA, Sharef YW, Al-Belushi AK, Al-Hashim H, Al-Ghailani M, et al. Hemorrhagic Cardioembolic Stroke Secondary to a Left Ventricular Thrombus: a Therapeutic Dilemma. Oman Med J. 2013;28:56-9. [CrossRef] [PubMed] [PMC free article]
- Beslow LA, Smith SE, Vossough A, Licht DJ, Kasner SE, Favilla CG, et al. Hemorrhagic Transformation of Childhood Arterial Ischemic Stroke. Stroke. 2011;42:941-6. [CrossRef] [PubMed] [PMC free article]
- Ferriero DM, Fullerton HJ, Bernard TJ, Billinghurst L, Daniels SR, DeBaun MR, et al. Management of Stroke in Neonates and Children: A Scientific Statement From the American Heart Association/American Stroke Association. Stroke [Internet]. 2019 Mar [cited 2019 Nov 18];50(3). Available from: https://www.ahajournals.org/doi/10.1161/STR.0000000000000183 [CrossRef] [PubMed]
- Birmingham E, Richardson RR. Rheumatic Fever and Rheumatic Heart Disease. In: Atlas of Acquired Cardiovascular Disease Imaging in Children [Internet]. Springer, Cham; 2017 [cited 2018 Feb 16]. p. 67-73. Available from: https://link.springer.com/chapter/10.1007/978-3-319-44115-3_11 [CrossRef]
- World Health Organization. Rheumatic fever and rheumatic heart disease [Internet]. WHO. [cited 2019 Nov 19]. Available from: https://www.who.int/cardiovascular_diseases/publications/trs923/en/
- Jordan LC, Hillis AE. Hemorrhagic Stroke in Children. Pediatr Neurol. 2007;36:73-80. [CrossRef] [PubMed] [PMC free article]
- Beslow LA, Abend NS, Gindville MC, Bastian RA, Licht DJ, Smith SE, et al. Pediatric Intracerebral Hemorrhage: Acute Symptomatic Seizures and Epilepsy. JAMA Neurol. 2013;70:448. [CrossRef] [PubMed] [PMC free article]
DOI: https://doi.org/10.7199/ped.oncall.2019.34
|
| Cite this article as: | | Tengkawan J, Karuniawaty T P, Ihyauddin Z, Septisari A A. Hemorrhagic Transformation of Embolic Stroke in Pediatric Rheumatic Heart Disease: A Case Report. Pediatr Oncall J. 2019;16: 119-121. doi: 10.7199/ped.oncall.2019.34 |
|